Your endometriosis pain has intensified recently. Flare-ups occur more frequently. You notice symptoms worsen on high pollution days. Could the air quality in your environment be aggravating your condition?
Understanding the Pollution-Endometriosis Connection
A 2023 comprehensive review published in BJOG (British Journal of Obstetrics and Gynaecology) examined how environmental pollution contributes to endometriosis onset and severity. The researchers emphasized that the interaction between pollution and endometriosis demands immediate attention as a pressing public health issue.
Endometriosis affects approximately 10% of women of reproductive age worldwide. This chronic gynecological disorder involves abnormal growth of endometrial tissue outside the uterus. These tissue growths can occur on ovaries, fallopian tubes, pelvic peritoneum, bladder, and intestines. The resulting symptoms include severe pelvic pain, painful periods, pain during intercourse, infertility, and compromised quality of life.
While endometriosis arises from a combination of genetic, hormonal, and environmental factors, pollution's influence has gained recognition as a significant contributor to disease development and progression. Environmental factors—particularly air pollution, water contamination, and occupational hazards—appear to play major roles in this complex condition.
How Air Pollution Triggers Endometriosis
Air pollution, specifically fine particulate matter (PM2.5) and polycyclic aromatic hydrocarbons (PAHs), associates with increased endometriosis risk through several biological mechanisms. These pollutants contain endocrine-disrupting chemicals (EDCs) that dysregulate hormonal balance, contributing to endometriosis progression.
PM2.5 particles penetrate deep into lungs and enter the bloodstream. Once circulating, these particles trigger systemic inflammation—a key driver of endometriosis development. The condition fundamentally involves chronic inflammatory processes. Environmental pollutants enhance this inflammation, creating conditions favorable for ectopic endometrial tissue growth and survival.
Polycyclic aromatic hydrocarbons found in air pollution possess estrogenic activity. These compounds can bind to and activate estrogen receptors throughout the body. Since endometriosis represents an estrogen-dependent disease, exposure to environmental estrogens potentially fuels lesion growth and symptom severity.
Oxidative stress represents another mechanism linking pollution to endometriosis. Air pollutants generate reactive oxygen species that damage cellular components including DNA, proteins, and lipids. This oxidative damage promotes inflammatory signaling and tissue dysfunction characteristic of endometriosis.
Chronic inflammation from pollution exposure also affects immune system function. The immune system normally removes ectopic endometrial cells. However, pollution-induced immune dysregulation may impair this protective mechanism, allowing endometrial implants to establish and proliferate outside the uterus.
What Research Documents
Multiple epidemiological studies examined associations between various pollution exposures and endometriosis diagnosis. A systematic review covering research from 2011-2016 found that several environmental toxicants significantly associated with reproductive disorders including endometriosis.
Research on bisphenol A (BPA)—a chemical found in plastics, epoxy resins, and numerous consumer products—revealed concerning patterns. The majority of studies showed women with endometriosis had higher BPA levels than women without the condition. BPA was detected in blood, serum, and follicular fluid at elevated concentrations in endometriosis patients.
However, some studies found no associations between serum BPA concentrations and endometriosis incidence. These conflicting results could reflect differences in study populations, sample sizes, exposure measurement methods, and endometriosis diagnostic approaches.
Phthalates—synthetic chemicals used in cosmetics, medications, and construction materials—also show connections to endometriosis. Several studies found that urinary metabolites of DEHP (a common phthalate) associated with endometriosis diagnosis. One study reported urinary levels of a specific DEHP metabolite were inversely associated with endometriosis risk, while another found no association.
Studies on dibutyl phthalate (DBP) reported that urinary MBP levels associated with nearly twofold increase in endometriosis diagnosis odds. Additionally, urinary and plasma DBP levels correlated with endometriosis. However, several other studies reported null associations between various phthalate metabolites and endometriosis.
The Dioxin Factor
Dioxins and dioxin-like compounds represent particularly concerning pollutants for endometriosis. These chemicals release into the environment as byproducts of combustion, chemical manufacturing, and metal industry operations. They persist in the environment and bioaccumulate in the food chain.
The Seveso Women's Health Study examined a unique population exposed to extremely high dioxin levels following a 1976 chemical explosion in Italy. This retrospective cohort assessed pregnancy outcomes and reproductive health over 30 years. Surprisingly, the study found no significant associations between maternal TCDD (a potent dioxin) exposure and endometriosis.
A Japanese study similarly found no significant association between serum dioxin levels and endometriosis in infertile women diagnosed with the condition. These null findings contrast with earlier research suggesting dioxin-endometriosis connections, highlighting ongoing scientific uncertainty.
Pesticides and Occupational Exposures
Organochlorine pesticides—persistent environmental pollutants—have been associated with increased endometriosis risk in some studies. These chemicals show bioaccumulation in fatty tissues and possess endocrine-disrupting properties affecting hormone signaling.
Occupational exposures to various chemicals may particularly impact endometriosis risk. Workers in industries using solvents, heavy metals, or other toxic substances face higher exposures than general populations. However, specific research on occupational pollution and endometriosis remains limited.
Water contamination represents another exposure route. Chemical contaminants including heavy metals, dioxins, and PCBs (polychlorinated biphenyls) in drinking water may disrupt hormonal regulation and potentially contribute to endometriosis development.
The Inflammation Connection
Endometriosis fundamentally involves chronic inflammation within the pelvic cavity. Ectopic endometrial tissue triggers immune responses that promote inflammatory cytokine production. This inflammatory environment supports lesion survival, angiogenesis (blood vessel formation), and nerve fiber growth contributing to pain.
Air pollution amplifies inflammatory processes throughout the body. PM2.5 exposure increases circulating inflammatory markers including C-reactive protein, interleukin-6, and tumor necrosis factor-alpha. For women with endometriosis, this systemic inflammation potentially exacerbates the localized pelvic inflammation driving symptoms.
The 2023 BJOG review emphasizes that air pollution enhances chronic inflammation, oxidative stress, and hormonal imbalances—all factors contributing to endometriosis progression. While the review provides compelling biological rationale, it acknowledges that more research specifically examining pollution's effects on endometriosis symptom severity remains needed.
Research Limitations and Conflicts
The evidence linking pollution to endometriosis faces several important limitations. Many studies show conflicting results. Some find significant associations while others report null findings. This inconsistency reflects challenges inherent in environmental health research.
Exposure assessment proves particularly difficult. Most studies rely on biomarker measurements at single time points. However, endometriosis develops over years. Past exposures during critical developmental windows may prove more relevant than current exposure levels. Without longitudinal exposure data, establishing causal relationships remains challenging.
Endometriosis diagnosis presents another complication. The gold standard requires surgical visualization and histological confirmation. Many women with symptoms never receive surgical diagnosis. This diagnostic uncertainty creates potential for misclassification bias in research studies.
Additionally, endometriosis involves multiple subtypes—superficial peritoneal lesions, ovarian endometriomas, and deep infiltrating endometriosis. These subtypes may respond differently to environmental exposures. Most studies don't differentiate between subtypes when examining pollution associations.
What This Means for Women With Endometriosis
If you have endometriosis, environmental factors are one modifiable factor that may affect your symptoms. While you cannot control outdoor pollution levels, you can improve indoor air quality where you spend most of your time.
Track your symptoms relative to air quality. Some women notice pain flares correlate with high pollution days. If patterns emerge, this information helps guide exposure reduction strategies and provides valuable information for healthcare discussions.
Reducing overall toxic burden makes biological sense given endometriosis involves inflammatory and hormonal mechanisms that pollution may worsen. Choose personal care products free from phthalates and parabens. Minimize plastic food container use to reduce BPA exposure. Filter drinking water to remove potential contaminants.
However, environmental interventions should complement rather than replace medical treatment. Endometriosis requires comprehensive management including hormonal therapies, pain management, and sometimes surgery. Environmental modifications represent additional tools rather than standalone solutions.
The Public Health Imperative
The 2023 review concludes that mitigating environmental pollution's impact is required to safeguard women's reproductive health. This requires comprehensive approaches involving stringent environmental regulations, sustainable practices, responsible waste management, research and innovation, public awareness, and collaboration among stakeholders.
Public health policies play major roles in addressing the pollution-endometriosis interaction as a long-term commitment. Individual actions alone cannot solve systemic environmental problems requiring regulatory and policy interventions.
As more research emerges connecting pollution to endometriosis and other gynecological conditions, the case for stronger environmental protections grows. Women's reproductive health deserves consideration when setting air quality standards and pollution regulations.
Protecting Yourself Through Clean Indoor Air
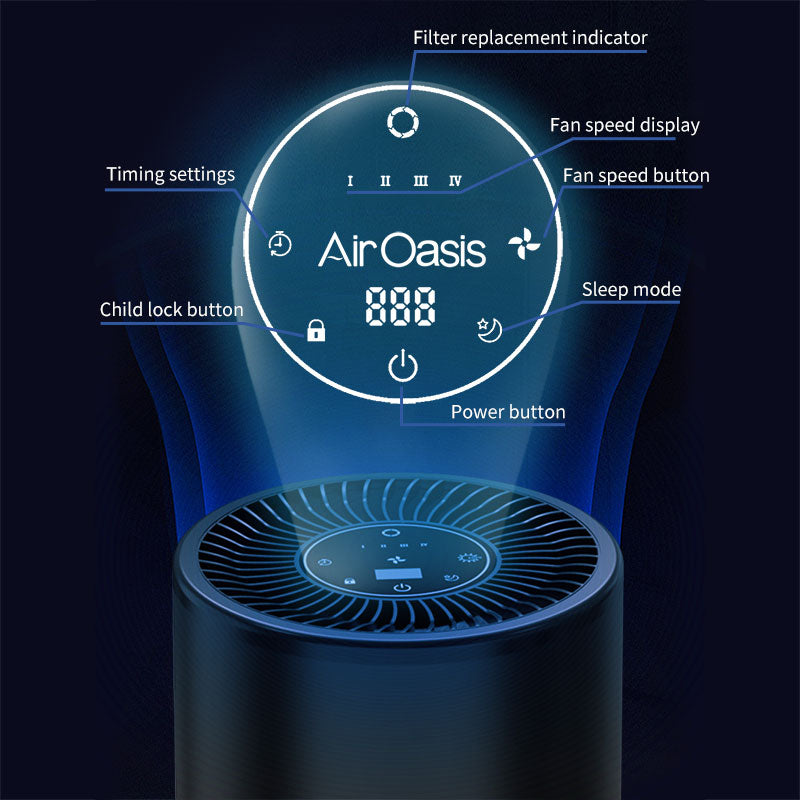
While outdoor pollution requires societal solutions, indoor air quality remains within individual control. Medical-grade air purification removes particulate matter and volatile organic compounds that research suggests may worsen endometriosis.
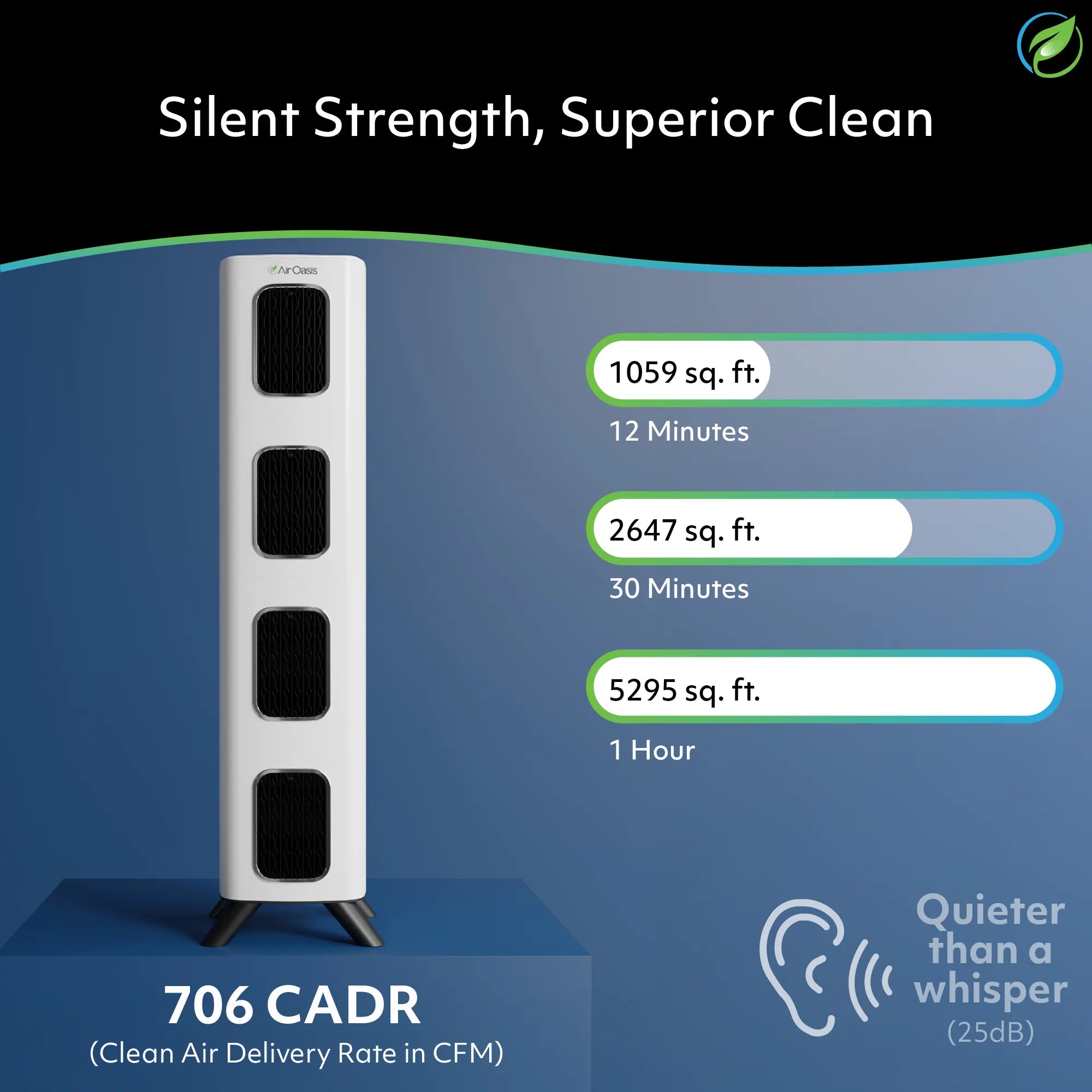
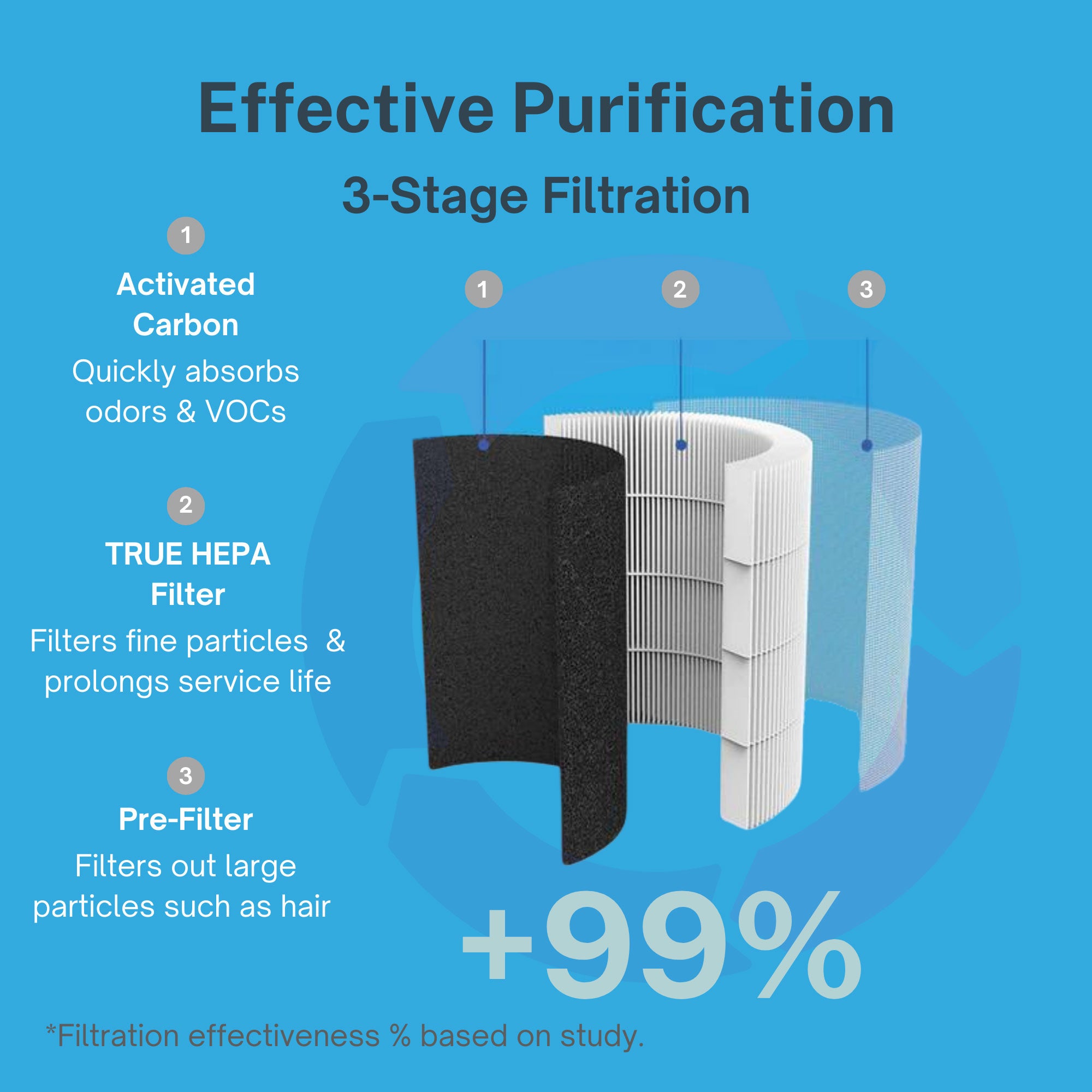
The iAdaptAir series provides comprehensive indoor air purification. HEPA filtration captures 99.97% of particles down to 0.3 microns including PM2.5 specifically linked to inflammatory diseases. Activated carbon removes volatile organic compounds and chemical pollutants. Multi-stage filtration addresses diverse indoor air quality threats.
Choose appropriate coverage for your living space. The iAdaptAir 2S purifies 265 sq ft, the 2M handles 530 sq ft, the 2L covers 795 sq ft, and the 2P serves 1,059 sq ft. Adequate air purification throughout your home reduces cumulative pollution exposure that may contribute to symptom flares.
The Path Forward
The connection between pollution and endometriosis represents an emerging research area requiring continued investigation. Current evidence suggests plausible biological mechanisms and some epidemiological support, but definitive proof requires additional well-designed studies.
Future research should examine whether reducing pollution exposure improves endometriosis symptoms in affected women. Longitudinal studies tracking exposure and symptoms over time would clarify temporal relationships. Research differentiating endometriosis subtypes could reveal whether certain lesion types show greater pollution sensitivity.
Until more definitive answers emerge, the precautionary principle applies. Reducing pollution exposure benefits health broadly beyond just potential endometriosis effects. Clean air supports respiratory, cardiovascular, and overall wellbeing.
If you have endometriosis, discuss environmental exposures with your healthcare provider. Consider air quality as one factor potentially affecting your condition. Take control where possible through indoor air purification and reduced toxic product use.
Protect your health through clean indoor air quality. Reducing pollution exposure may help manage endometriosis symptoms while providing numerous other health benefits. Shop Air Oasis today and create the pristine environment your body needs to heal.