Your nose houses an invisible ecosystem of fungi that scientists are just beginning to understand. Groundbreaking research from the University of Porto reveals that people suffering from allergic rhinitis have fundamentally different fungal communities living in their nasal passages compared to healthy individuals. This discovery opens new pathways for understanding and potentially treating the chronic sniffles, sneezing, and congestion that plague nearly a quarter of adults worldwide.
Understanding the Nasal Mycobiome
The mycobiome refers to the community of fungi living in and on your body. While bacteria receive most attention in microbiome research, fungi play equally important roles in human health. Your nasal passages provide home to numerous fungal species that exist in delicate balance with your immune system.
Dr. Luís Delgado and his research team studied 214 children and young adults attending an immunology and asthma clinic in Porto, Portugal. They compared nasal swab samples from patients with allergic rhinitis and asthma to samples from healthy controls. The differences proved striking and statistically significant.
Patients with allergic rhinitis displayed significantly higher fungal diversity in their noses compared to healthy people. Their nasal passages hosted richer, more varied fungal communities. This increased diversity suggests that chronic respiratory inflammation disrupts the normal mycobiome balance, creating conditions where more fungal species can colonize nasal tissue.
The most common fungal families found across all samples belonged to Ascomycota and Basidiomota. Within these families, 14 genera dominated the nasal mycobiomes. Many of these fungi are recognized as allergenic or opportunistic pathogens in humans. This discovery positions the nasal cavity as a major reservoir for fungi potentially involved in allergic rhinitis and asthma development.
The Allergy-Asthma Connection
Allergic rhinitis causes sneezing, itching, inflamed nasal membranes, and a blocked, runny nose. These symptoms disrupt sleep, reduce productivity, and significantly impact quality of life. Nearly a quarter of Portuguese adults suffer from this condition, with similar prevalence rates worldwide.
Allergic rhinitis frequently occurs alongside asthma. Both conditions involve inflammation and airway obstruction. Some researchers believe they represent different manifestations of the same underlying airway inflammatory disease. Understanding their connection becomes critical for developing effective treatments.
The Porto research team found no significant mycobiome differences between patients who had only allergic rhinitis, only asthma, or both conditions together. All three groups showed similarly altered fungal communities compared to healthy controls. This suggests the mycobiome disruption relates to chronic respiratory inflammation generally rather than specific disease presentations.
Interestingly, patients with both allergic rhinitis and asthma showed more evidence of fungal interactions in their nasal passages. The fungi in these patients' noses demonstrated stronger connections between different species. This network of fungal relationships could indicate that the fungi actively affect the nose's immune environment, potentially worsening inflammation and symptoms.
Metabolic Pathways and Future Treatment Targets
The research revealed intriguing metabolic differences in patients' nasal mycobiomes. Three metabolic pathways associated with producing 5-aminoimidazole ribonucleotide, or AIR, appeared overabundant in patients with allergic rhinitis and asthma.
AIR serves as a building block for DNA and RNA synthesis. It links to purine production, which cells need for energy metabolism and genetic material construction. The overabundance of AIR-related pathways in allergic rhinitis patients suggests fungal metabolism may contribute to disease processes.
If future research confirms this connection and identifies the exact mechanisms, AIR could become a therapeutic target. Doctors might diagnose mycobiome problems before clinical symptoms appear. Treatments could potentially modulate fungal metabolism to reduce inflammation and alleviate symptoms.
However, the researchers acknowledge study limitations. They couldn't control all patient-specific variables including disease severity and treatment levels. The cross-sectional design provides a snapshot at one point in time rather than tracking how mycobiomes change over disease progression.
Longitudinal studies following patients over months or years would reveal whether fungi drive disease processes or simply respond to inflammation created by other causes. Such research could identify which specific fungi contribute most to symptom development and disease severity.
Indoor Air Quality and Nasal Mycobiomes
Your nasal mycobiome doesn't exist in isolation from your environment. The air you breathe constantly introduces new fungal spores to your nasal passages. Indoor air quality directly influences which fungi colonize your nose and how abundantly they grow.
Mold growth in homes releases massive quantities of spores into indoor air. Damp conditions, water damage, and poor ventilation create ideal mold growth environments. When you breathe mold-contaminated air, those spores settle in your nasal passages where some establish colonies.
People with allergic rhinitis may be particularly vulnerable to environmental fungal exposure. Their already inflamed nasal tissues provide disrupted environments where diverse fungi colonize more easily. Reducing indoor mold exposure could potentially help restore healthier mycobiome balance.
Dust accumulation harbors fungal spores. Carpeting, upholstery, and bedding collect spores that become airborne again with normal household activity. Poor indoor air circulation allows fungal spores to accumulate at higher concentrations than would occur with proper ventilation and air cleaning.
HVAC systems can either help or harm nasal mycobiome health. Clean, well-maintained systems with effective filtration reduce fungal spore circulation. Contaminated systems with moldy ductwork actually distribute spores throughout homes, increasing occupant exposure.
Protecting Your Respiratory Health
While researchers work toward mycobiome-based treatments for allergic rhinitis and asthma, you can take action now to reduce environmental fungal exposure. Controlling indoor air quality represents your most direct defense against problematic fungal colonization.
Address moisture problems immediately. Fix leaks, improve ventilation in bathrooms and kitchens, and use dehumidifiers in damp areas. Mold can't grow without moisture. Maintaining indoor relative humidity between 30-50% prevents most mold growth.
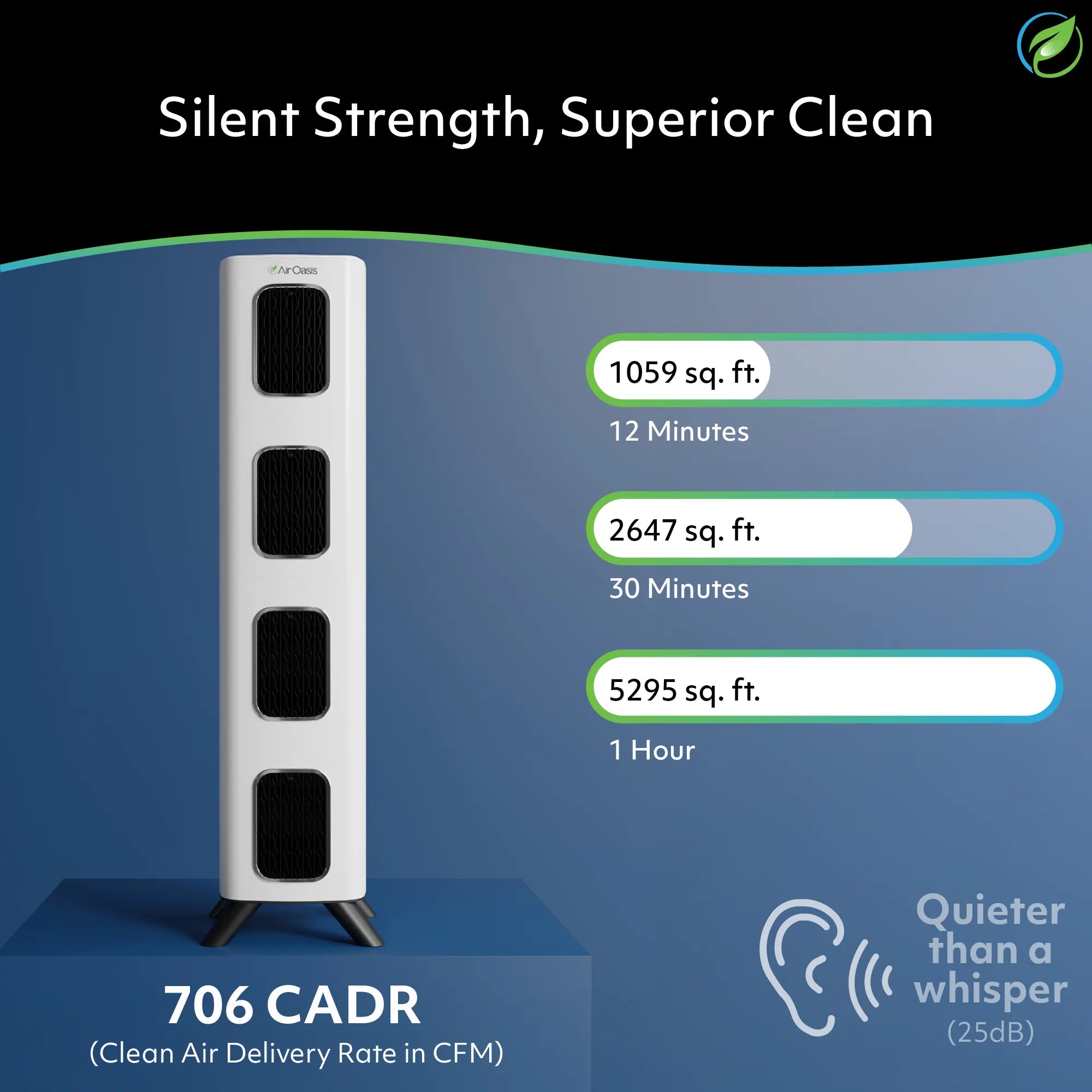
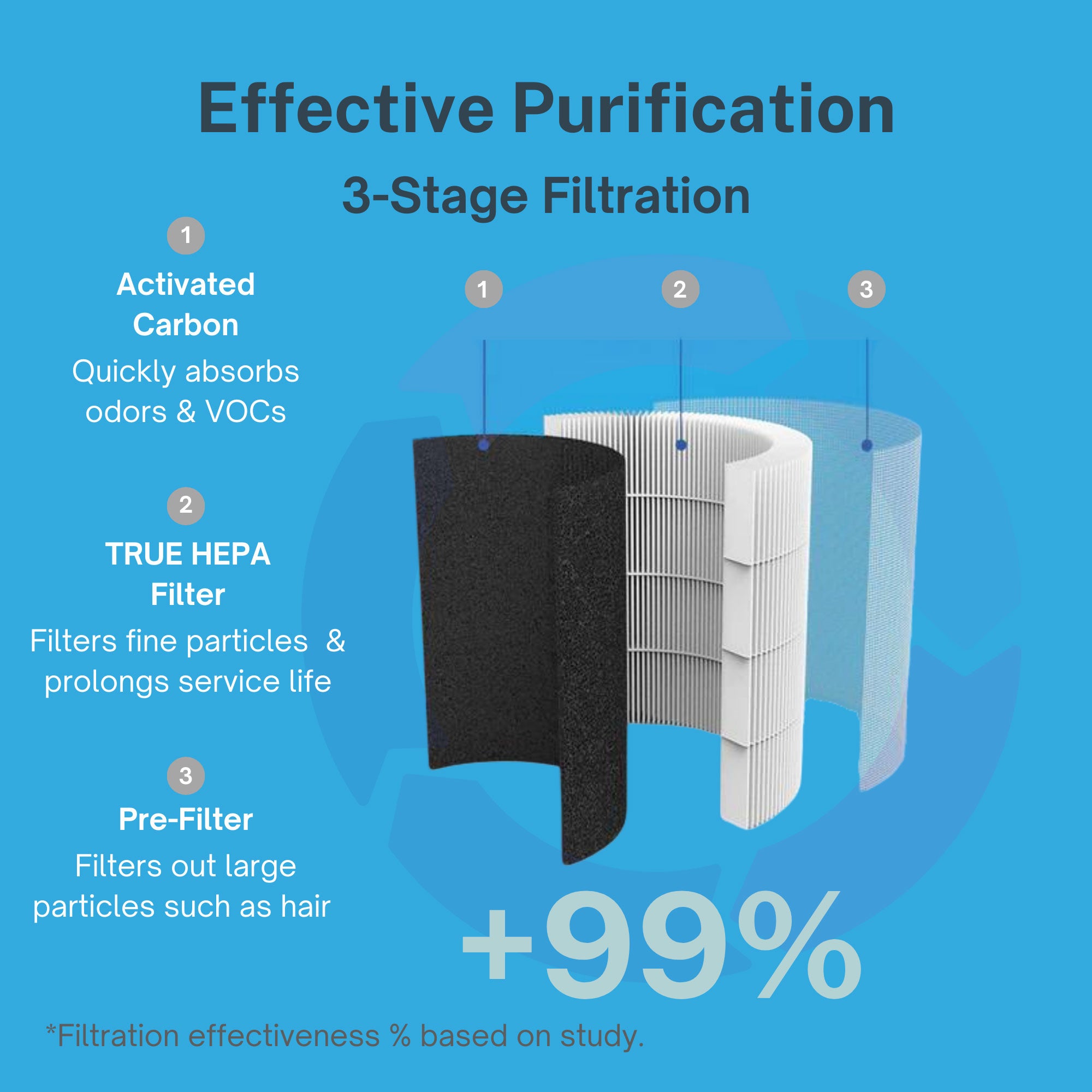
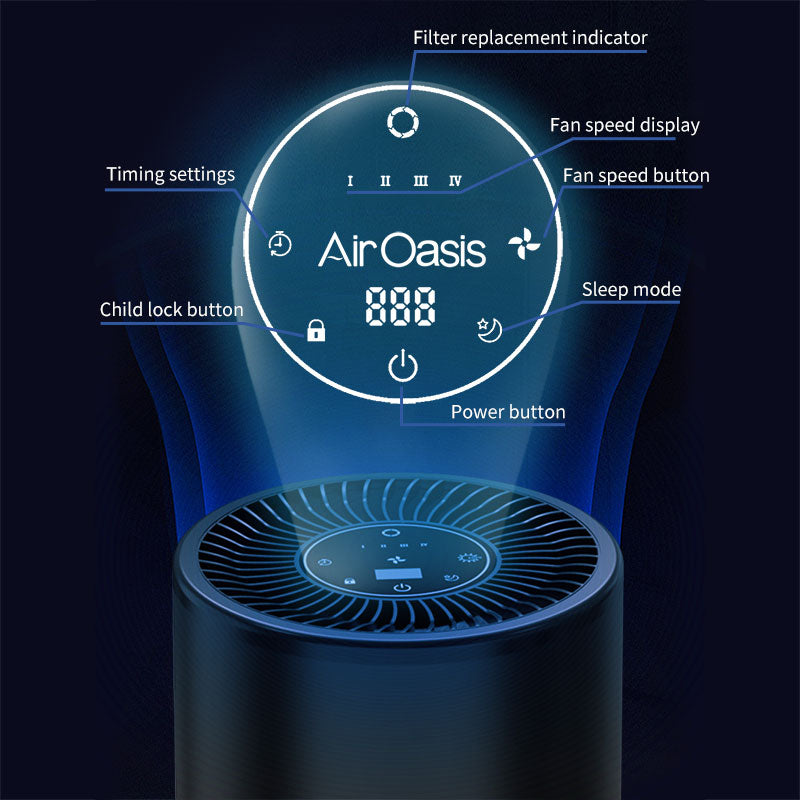
Medical-grade air purification removes airborne fungal spores before they reach your nasal passages. True HEPA filtration captures mold spores, pollen, and other particulates that trigger allergic responses. Activated carbon filters absorb volatile organic compounds released by fungal growth. UV-C technology neutralizes captured spores, preventing them from reproducing.
Regular cleaning reduces fungal reservoirs in your home. Vacuum with HEPA-filtered vacuum cleaners to avoid redistributing spores into air. Wash bedding weekly in hot water. Clean bathroom and kitchen surfaces prone to moisture accumulation.
Monitor your symptoms in relation to indoor environments. Many people notice their allergic rhinitis worsens in certain locations or seasons. These patterns often reflect fungal exposure variations. Identifying problem environments helps you take targeted action.
The Future of Mycobiome Research
The Porto study opens fascinating research directions. Scientists now have evidence that nasal mycobiomes differ fundamentally between healthy people and those with chronic respiratory inflammation. This knowledge creates opportunities for novel diagnostic approaches and treatment strategies.
Future research may identify specific fungal species most strongly associated with severe symptoms. Treatments could target those species specifically rather than using broad-spectrum approaches. Probiotics containing beneficial fungi might help restore healthy mycobiome balance in diseased nasal passages.
Personalized medicine approaches might analyze individual patients' nasal mycobiomes to guide treatment selection. Some patients might benefit from antifungal therapies while others need anti-inflammatory treatments or allergen immunotherapy. Mycobiome analysis could predict which approach works best for each person.
The connection between environmental exposure and nasal colonization deserves deeper investigation. Understanding how indoor air quality affects mycobiome composition could lead to environmental interventions that prevent allergic rhinitis development or reduce symptom severity.
Taking Control of Your Nasal Health
You can't change your nasal mycobiome directly today. Research hasn't progressed to clinical treatments yet. You can reduce environmental fungal exposure that influences which fungi colonize your nose and how abundantly they grow.
Clean indoor air reduces the constant influx of fungal spores that challenge your nasal passages. For people with allergic rhinitis and asthma, this reduction could ease symptoms and potentially help restore healthier mycobiome balance over time.
Your respiratory health depends on every breath. When that air contains high concentrations of fungal spores, your nasal passages struggle to maintain healthy conditions. Medical-grade air purification provides proven protection against environmental fungi that research now links to chronic respiratory disease.
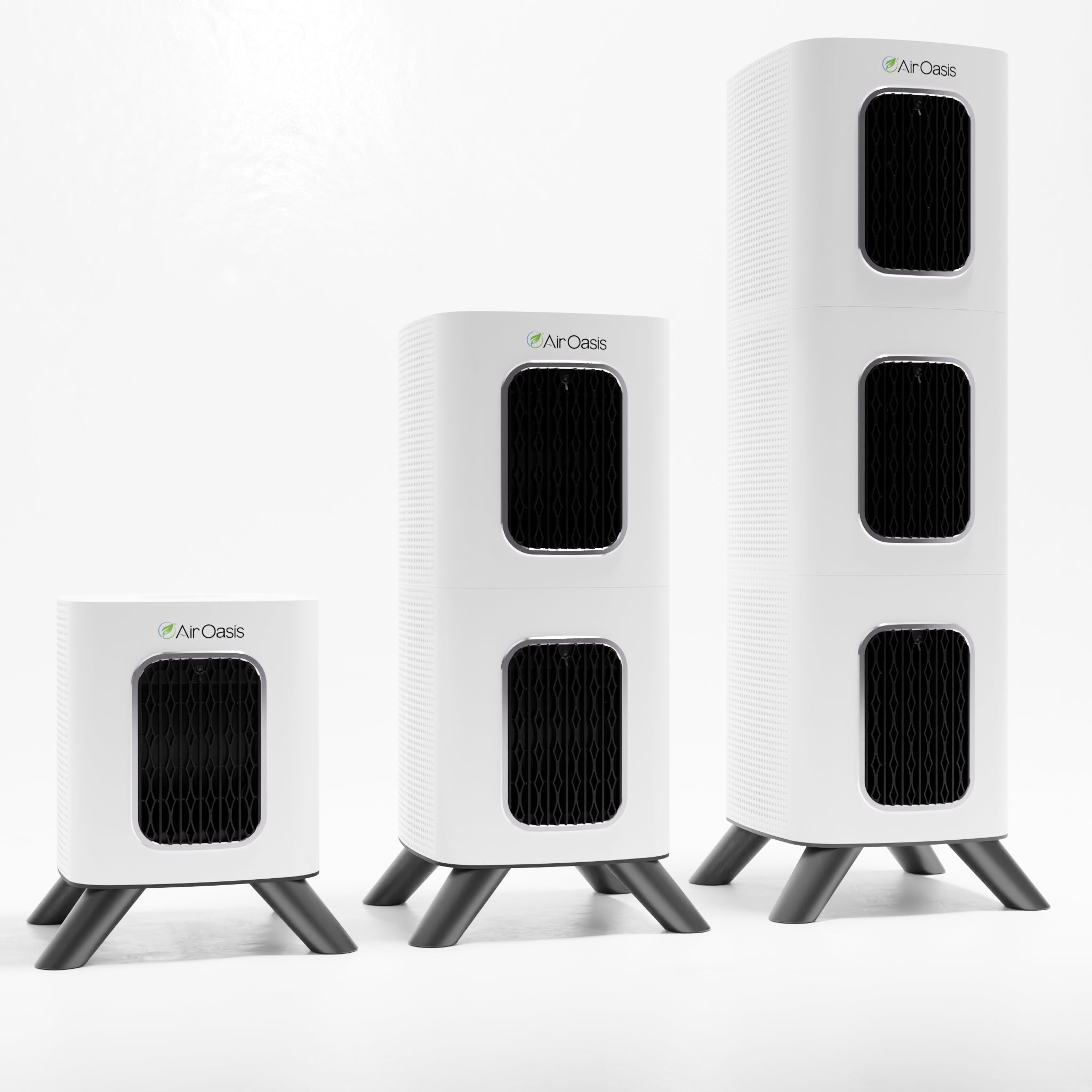
Ready to reduce fungal exposure and support your respiratory health? Advanced air purification removes mold spores and other airborne fungi before they reach your nasal passages. Shop Air Oasis today and breathe cleaner air that supports rather than challenges your nasal mycobiome.