Patients battling chronic Lyme disease often face a frustrating reality: despite months or years of antibiotic treatment, their symptoms persist or return with alarming regularity. While medical professionals debate treatment protocols and testing methods, a growing body of evidence points to an overlooked factor that may explain treatment failures—Chronic Inflammatory Response Syndrome (CIRS) caused by mold and biotoxin exposure.
This hidden connection between environmental toxins and infectious disease recovery represents a paradigm shift in understanding why some Lyme patients achieve full recovery while others remain chronically ill despite aggressive treatment approaches.
The Shared Inflammatory Pathway Problem
Both CIRS and Lyme disease trigger identical inflammatory cascades within the immune system, creating a biological perfect storm that can trap patients in chronic illness cycles. The conditions share dysregulated cytokine production, particularly pro-inflammatory proteins that normally help fight infections but become destructively overactive in both diseases.
According to research published in Frontiers in Cellular and Infection Microbiology, mold exposure significantly weakens immune system function, reducing the body's ability to mount effective responses against bacterial infections like Lyme disease. This immunosuppressive effect can increase Lyme disease susceptibility by up to 40% in exposed individuals.
The inflammatory pathways activated by both conditions create overlapping symptoms that make differential diagnosis challenging. Patients experience cognitive dysfunction, chronic fatigue, joint pain, neurological symptoms, and mood disturbances regardless of whether mold toxins, Lyme bacteria, or both are driving their illness. This symptom overlap often leads to incomplete treatment approaches that address only one condition while allowing the other to perpetuate systemic inflammation.
When both conditions coexist, they create synergistic effects that amplify each other's impact, making recovery significantly more difficult than treating either condition alone.
The Immune System Vulnerability Cycle
Lyme disease creates specific vulnerabilities that make patients more susceptible to developing CIRS from subsequent mold exposure. The bacterial infection disrupts normal immune regulation, compromises gut barrier function, and depletes the body's natural detoxification resources, creating ideal conditions for biotoxin accumulation.
Conversely, patients with existing CIRS face increased risks of developing severe Lyme disease if exposed to tick-borne infections. The chronic inflammation from mold exposure impairs immune surveillance mechanisms, reduces antimicrobial peptide production, and creates systemic conditions that allow bacterial infections to establish persistent reservoirs throughout the body.
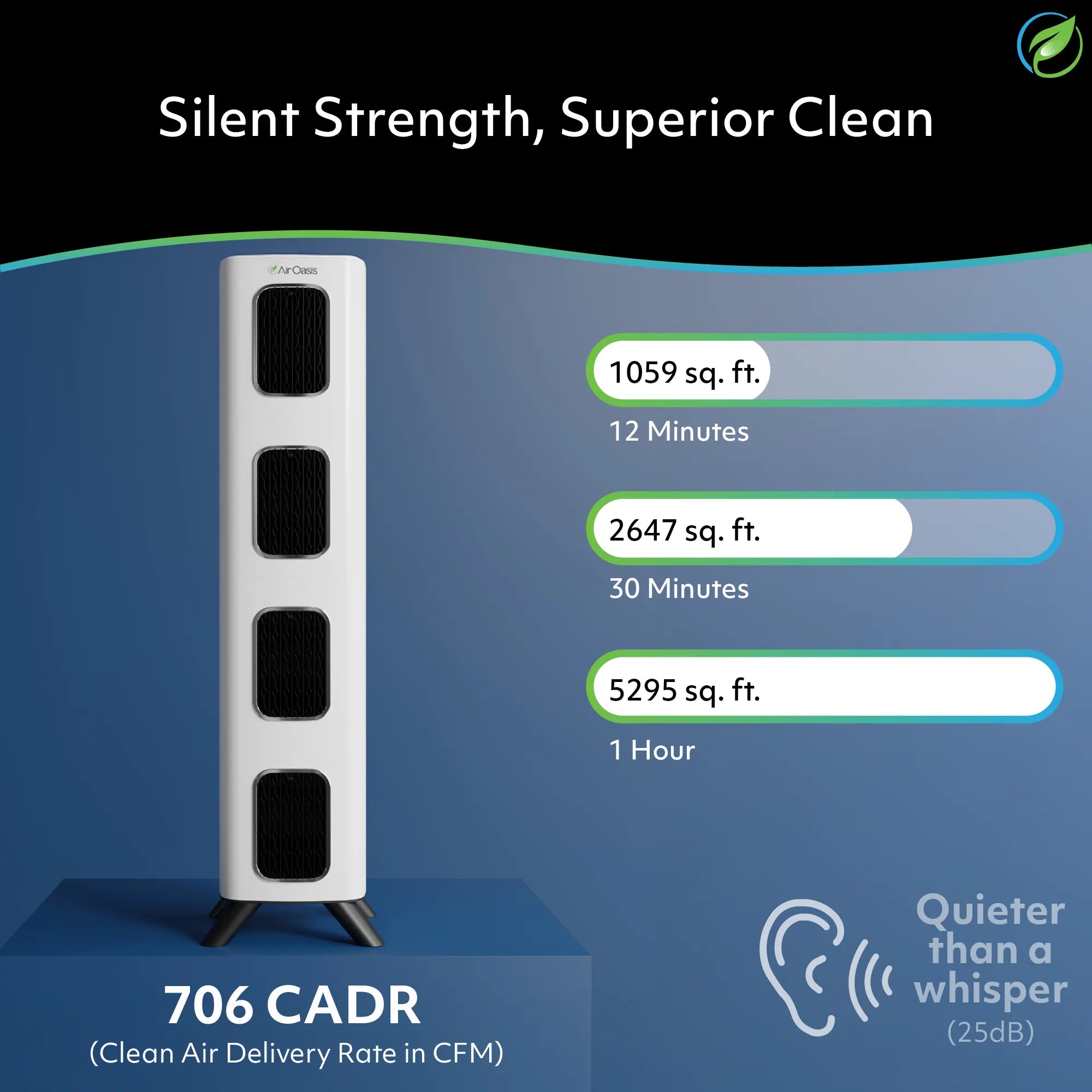
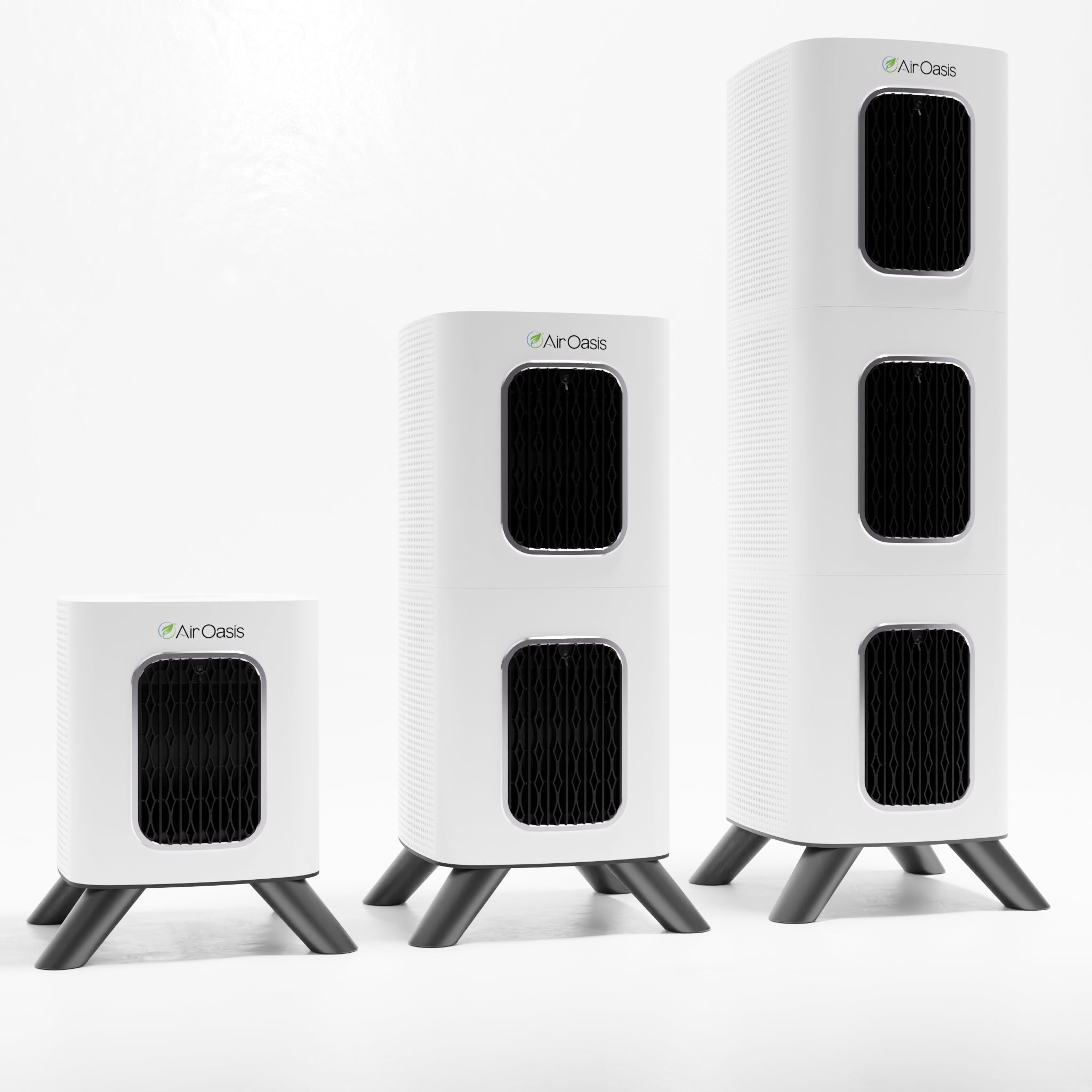
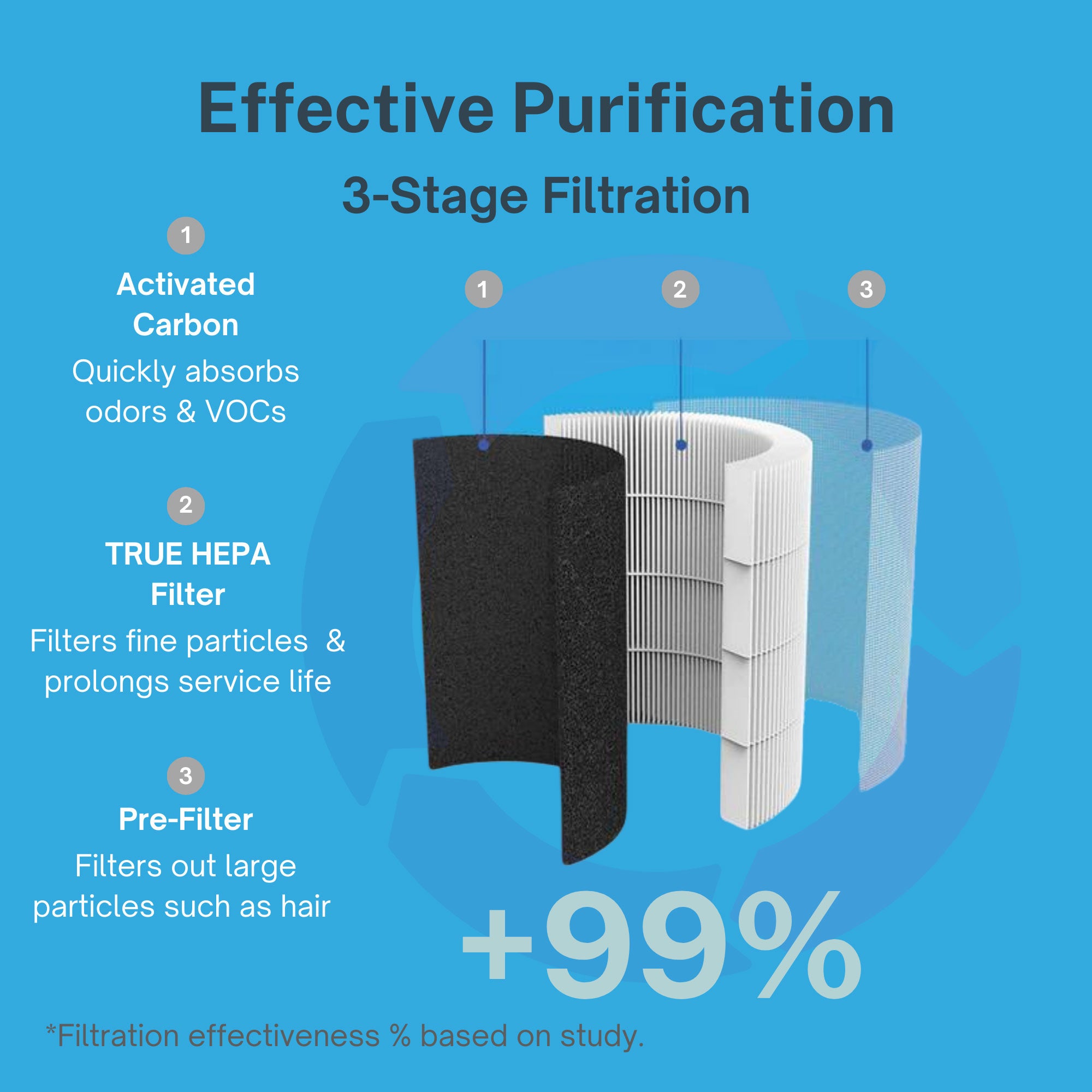
The Air Oasis focus on comprehensive environmental protection addresses this vulnerability by preventing the mold exposure that can trigger CIRS development in immunocompromised patients dealing with chronic infections.
This bidirectional relationship explains why patients with one condition often develop the other, creating compound health challenges that resist conventional single-pathogen treatment approaches. Breaking this cycle requires addressing environmental factors alongside infectious disease treatment.
Biotoxin Accumulation: The Hidden Treatment Barrier
The presence of biotoxins from mold exposure creates a biological barrier that prevents effective Lyme disease treatment by overwhelming the body's detoxification pathways. Mycotoxins from mold compete with bacterial endotoxins from Lyme for the same elimination routes, creating toxic accumulation that perpetuates inflammation regardless of antibiotic effectiveness against the bacterial infection.
Research from the National Institute of Environmental Health Sciences demonstrates that biotoxin exposure creates long-lasting immune dysfunction that persists even after removing the source of exposure. In Lyme patients, this means that historical mold exposure can continue affecting treatment outcomes long after changing environments.
The biotoxin burden also affects medication metabolism and distribution, potentially reducing antibiotic effectiveness while increasing side effect risks. Patients may experience treatment intolerance that physicians interpret as treatment failure when the real issue involves biotoxin interference with normal drug processing.
Comprehensive biotoxin elimination becomes essential for restoring the physiological conditions necessary for successful infectious disease treatment, yet this environmental component rarely receives attention in conventional Lyme disease protocols.
The Gut-Brain-Immune Connection
Both CIRS and Lyme disease devastate the gastrointestinal system, creating cascading effects that impact brain function and immune regulation. Mold mycotoxins directly damage intestinal mucosa while Lyme bacteria disrupt the microbiome and compromise gut barrier integrity, creating conditions for increased intestinal permeability and systemic inflammation.
The damaged gut environment allows bacterial translocation, food sensitivities, and nutrient malabsorption that further compromise immune function and neurological health. This gut dysfunction explains many of the neuropsychiatric symptoms shared between CIRS and Lyme disease, including depression, anxiety, cognitive impairment, and mood instability.
The Air Oasis commitment to removing airborne toxins that contribute to gut inflammation recognizes the interconnected nature of environmental health and systemic wellness. Reducing toxic load through comprehensive air purification supports gut healing and immune system recovery.
Addressing gut health becomes crucial for breaking the inflammatory cycle that perpetuates both conditions, yet conventional treatment approaches often overlook this foundational aspect of recovery.
Geographic and Seasonal Patterns
Understanding the geographic overlap between Lyme disease endemic areas and regions with high mold exposure risks helps explain treatment outcome variations across different locations. Areas with high humidity, frequent flooding, or older housing stock create increased risks for both tick exposure and building-related mold problems.
Seasonal patterns also influence the relationship between these conditions. Spring and summer increase tick exposure risks while also creating ideal conditions for mold growth through increased humidity and storm-related water damage. Patients may experience symptom exacerbations during these periods due to combined exposure risks rather than simple disease progression.
Climate change effects on both tick populations and extreme weather events that promote mold growth suggest this dual exposure risk will continue increasing, making environmental awareness even more critical for patients in endemic areas.
Recognition of these environmental factors helps explain why some geographic regions report higher rates of treatment-resistant Lyme disease and supports the need for comprehensive environmental assessment in affected patients.
Treatment Integration Strategies
Successful management of patients with both CIRS and Lyme disease requires integrated treatment approaches that address environmental factors before, during, and after infectious disease treatment. This means comprehensive mold assessment and remediation must precede antimicrobial therapy for optimal outcomes.
The treatment sequence typically involves environmental testing and remediation, biotoxin binding and elimination, immune system support and inflammation reduction, targeted antimicrobial therapy for Lyme disease, and ongoing environmental maintenance to prevent recurrence. Each phase builds upon the previous one, with environmental control providing the foundation for all subsequent interventions.
Monitoring both infectious disease markers and CIRS-specific inflammatory parameters provides objective measures of treatment progress while helping identify which aspects of the combined illness require additional attention.
Long-term success requires understanding that genetic susceptibilities to biotoxins don't disappear with treatment, making ongoing environmental vigilance a permanent lifestyle requirement rather than a temporary intervention.
The Path Forward: Environmental Medicine Integration
The growing recognition of CIRS-Lyme connections represents a shift toward environmental medicine approaches that consider the complex interactions between genetic susceptibility, environmental exposures, and infectious diseases. This integrated perspective offers hope for patients who've exhausted conventional treatment options without achieving sustained recovery.
Success requires moving beyond single-pathogen treatment models toward comprehensive approaches that address the environmental factors perpetuating chronic illness. This shift demands collaboration between infectious disease specialists, environmental medicine practitioners, and building science professionals to create truly effective treatment protocols.
Patient education about environmental health becomes essential for empowering individuals to take control of factors that directly impact their recovery potential and long-term health maintenance.
Your Environment Shapes Your Recovery
Don't let hidden environmental factors undermine your healing journey. Take control of your indoor air quality with proven technology that removes the mold spores, mycotoxins, and biotoxins that could be preventing your complete recovery. Shop Air Oasis today for comprehensive air purification that supports your path to lasting wellness.