You slept eight hours but wake up exhausted. You struggle to concentrate at work. You need an afternoon nap just to function. Your energy levels have plummeted, but you're not sick—you just have allergies. The connection between sneezing and overwhelming fatigue puzzles many allergy sufferers. But the exhaustion is real, and the biological mechanisms causing it are well-documented.
Your Immune System Runs on Energy
Allergic reactions trigger a full immune system response. Your body produces immunoglobulin E antibodies that attach to mast cells. When allergens bind to these antibodies, mast cells release histamine and dozens of other inflammatory chemicals. This cascade requires significant metabolic energy.
Your immune system treats allergens like dangerous invaders. It mobilizes resources to fight perceived threats. This heightened alert state quickly depletes energy reserves. You feel tired because your body is genuinely working hard at the cellular level to respond to allergens.
Inflammation throughout your body accelerates energy consumption. Inflamed nasal passages, irritated airways, and swollen sinus tissue all require extra blood flow and cellular activity. Your cardiovascular system works harder to deliver oxygen and nutrients to inflamed tissues. This increased demand depletes your energy.
Cytokines, the signaling molecules your immune system releases during allergic reactions, directly cause fatigue. These proteins communicate between immune cells to coordinate responses. They also affect your brain, inducing feelings of tiredness and lethargy. It's a protective mechanism—your body wants you to rest so it can focus resources on fighting perceived threats.
Sleep Quality Plummets During Allergy Attacks
Nasal congestion disrupts breathing during sleep. You can't breathe through your nose, so you mouth-breathe all night. This causes dry mouth, snoring, and frequent waking. You might think you slept eight hours, but your sleep quality was terrible.
Postnasal drip triggers coughing that wakes you repeatedly throughout the night. Each coughing fit interrupts your sleep cycle. You never reach the deep restorative sleep stages your body needs for physical recovery and energy restoration.
Allergy symptoms often worsen at night when you lie down. Sinus drainage changes in horizontal positions. Dust mite exposure peaks in bedding. You spend hours trying to find comfortable sleeping positions while your nose is stuffy and your throat itches. This restlessness prevents the continuous, uninterrupted sleep necessary for feeling rested.
Sleep apnea worsens with nasal congestion from allergies. Blocked airways cause breathing pauses during sleep that drop your blood oxygen levels. You wake gasping for air, even if you don't fully remember these episodes. Your brain and body are starved of oxygen repeatedly throughout the night, leaving you exhausted by morning.
Antihistamines Contribute to Drowsiness
First-generation antihistamines like diphenhydramine and chlorpheniramine cross the blood-brain barrier. They block histamine receptors in your brain that help maintain wakefulness and alertness. This creates the drowsiness that makes these medications effective sleep aids but terrible for daytime allergy management.
Even newer non-drowsy antihistamines affect some people. While they're designed to avoid brain penetration, individual responses vary. You might experience fatigue from medications marketed as non-sedating simply because your body processes them differently than the average person.
Taking multiple allergy medications compounds fatigue effects. Antihistamines plus decongestants plus nasal steroids may control symptoms, but can leave you feeling drugged and lethargic. The combination of medication side effects and underlying allergic inflammation creates overwhelming tiredness.
Chronic Inflammation Drains Your Reserves
Allergies aren't just acute episodes—they create ongoing inflammation when you're exposed to triggers daily. Year-round allergies to dust mites, pet dander, or mold mean your immune system is constantly in a heightened state of alert. This chronic activation exhausts your body's resources over time.
Inflammatory compounds affect your brain directly. They can cross the blood-brain barrier and influence neurotransmitter function. This contributes to brain fog, difficulty concentrating, and the mental fatigue that makes thinking feel effortful during allergy flares.
Chronic sinus inflammation prevents proper oxygen exchange. When your sinuses are swollen and mucus-filled, air can't circulate efficiently through your nasal passages. This reduces oxygen intake with every breath. Your brain and muscles receive less oxygen than they need for optimal function, contributing to physical and mental fatigue.
Dehydration Compounds the Problem
Allergy symptoms cause fluid loss. Runny noses drain fluids. Watery eyes leak tears constantly. Post-nasal drip requires frequent swallowing and spitting. This fluid loss leads to mild dehydration that intensifies fatigue.
Antihistamines and decongestants have drying effects that worsen dehydration. They reduce mucus production but also decrease overall body moisture. When you're dehydrated, your blood volume drops slightly. Your heart must work harder to circulate blood, and your cells function less efficiently. You feel tired, sluggish, and weak.
Mouth breathing from nasal congestion dries out your mouth and throat overnight. You wake dehydrated after eight hours of losing moisture through your open mouth. This morning, dehydration adds to the fatigue you already feel from poor sleep quality and immune system activation.
Breaking the Fatigue Cycle
Address the root cause—allergen exposure—rather than just treating symptoms. Reducing contact with triggers decreases immune system activation. Less inflammation means less energy drain and better sleep quality. Environmental control provides benefits that medications alone cannot deliver.
Improve sleep quality by controlling allergens in the bedroom. Wash bedding weekly in hot water. Use allergen-proof mattress and pillow covers. Keep humidity below 50 percent to discourage dust mites. These steps reduce nighttime allergen exposure that disrupts sleep and triggers inflammation.
Stay hydrated throughout the day to counter fluid losses from allergy symptoms and medication effects. Drink water regularly, even if you don't feel thirsty. Proper hydration helps your body function more efficiently and reduces the fatigue associated with fluid depletion.
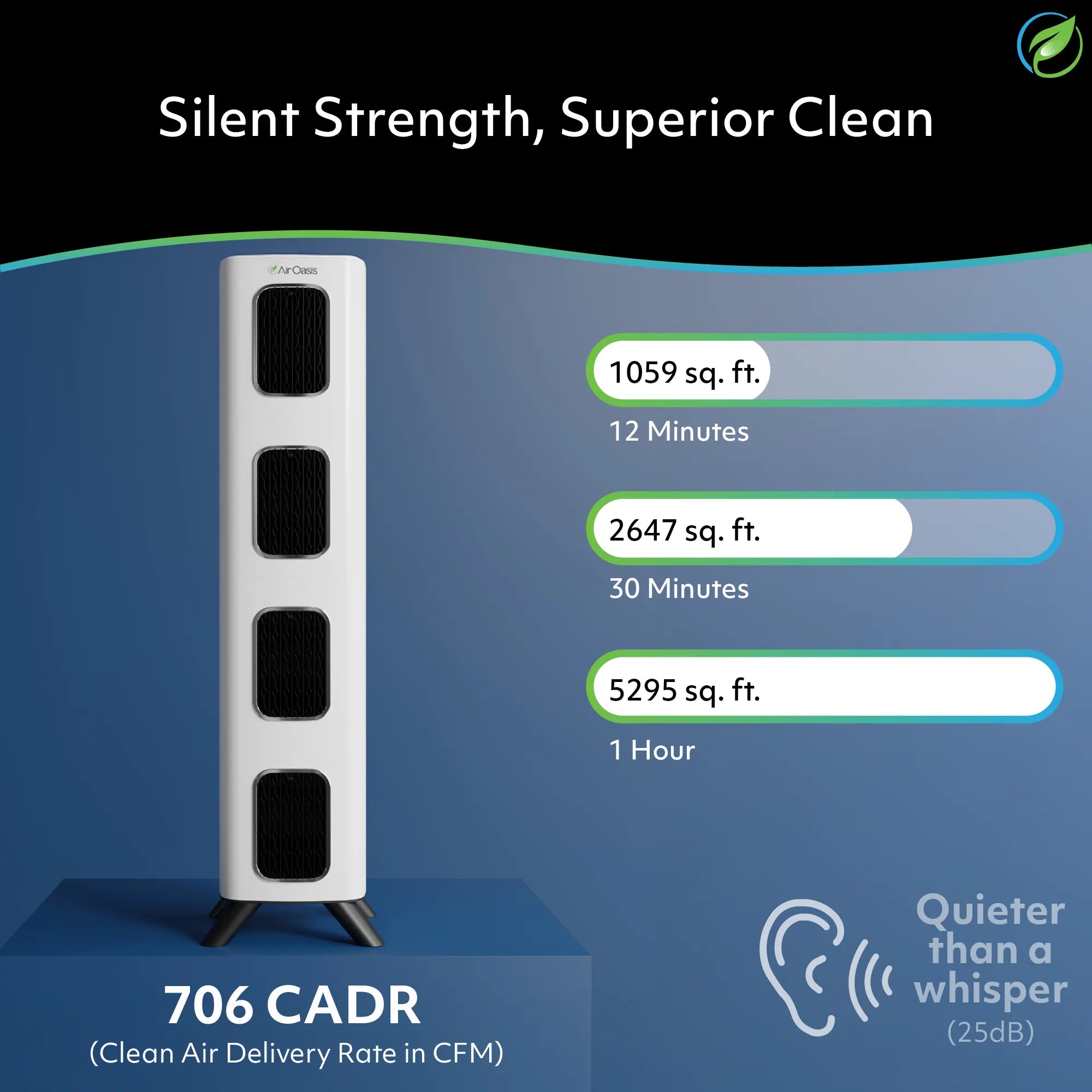
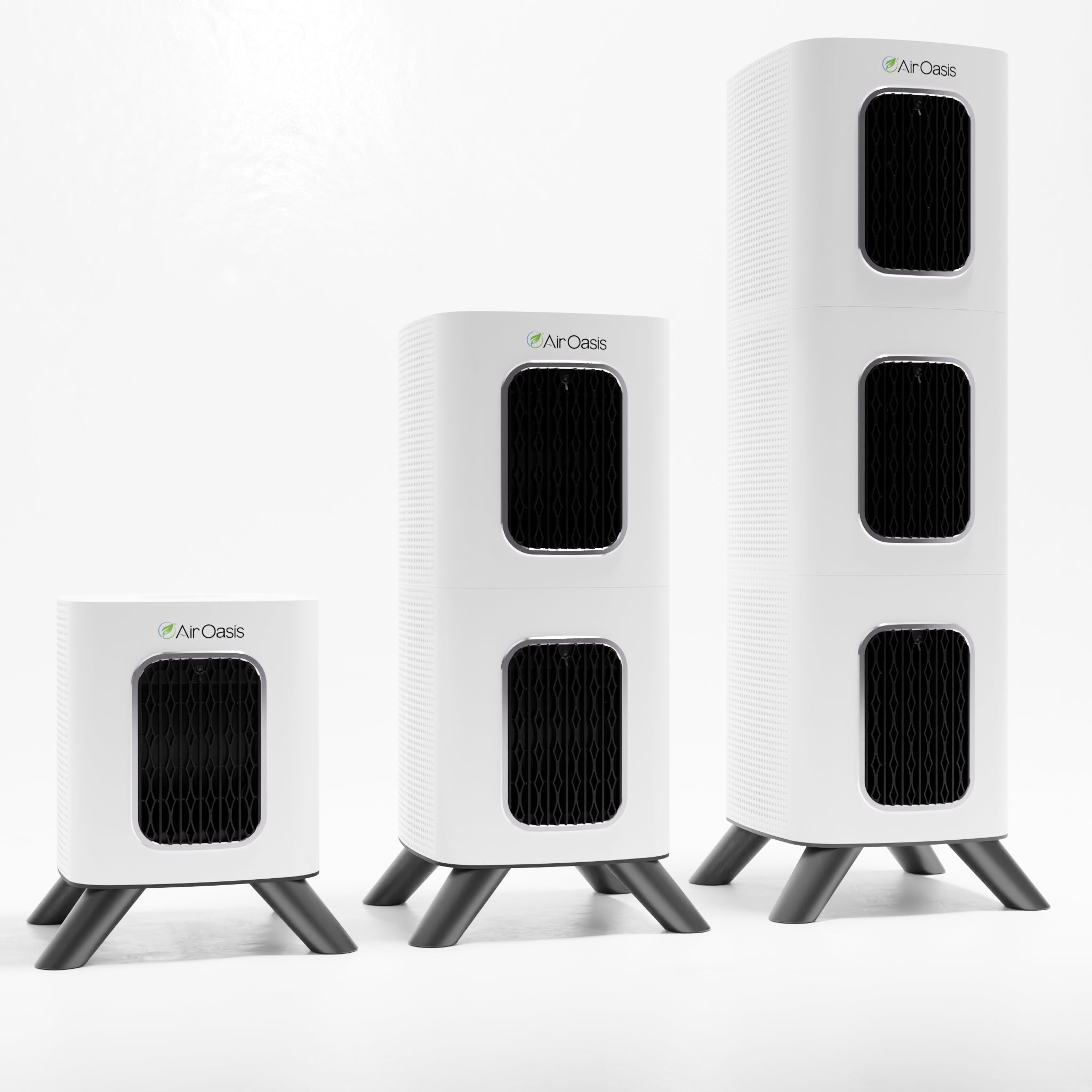
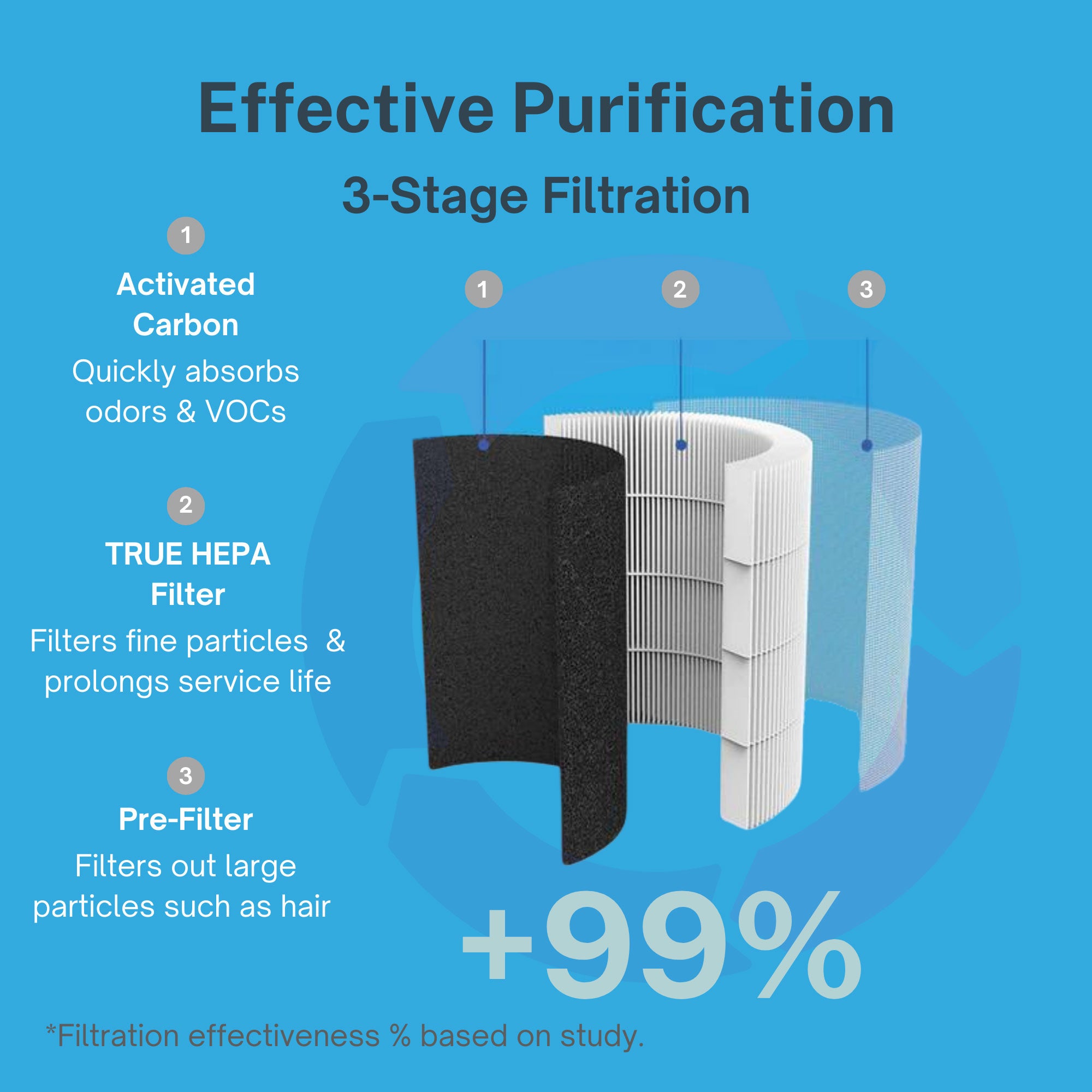
Medical-grade air purification removes allergens before they trigger immune responses. When you breathe cleaner air with fewer pollen particles, dust mites, pet dander, and mold spores, your immune system doesn't need to work as hard. Less immune activation means more energy for you.
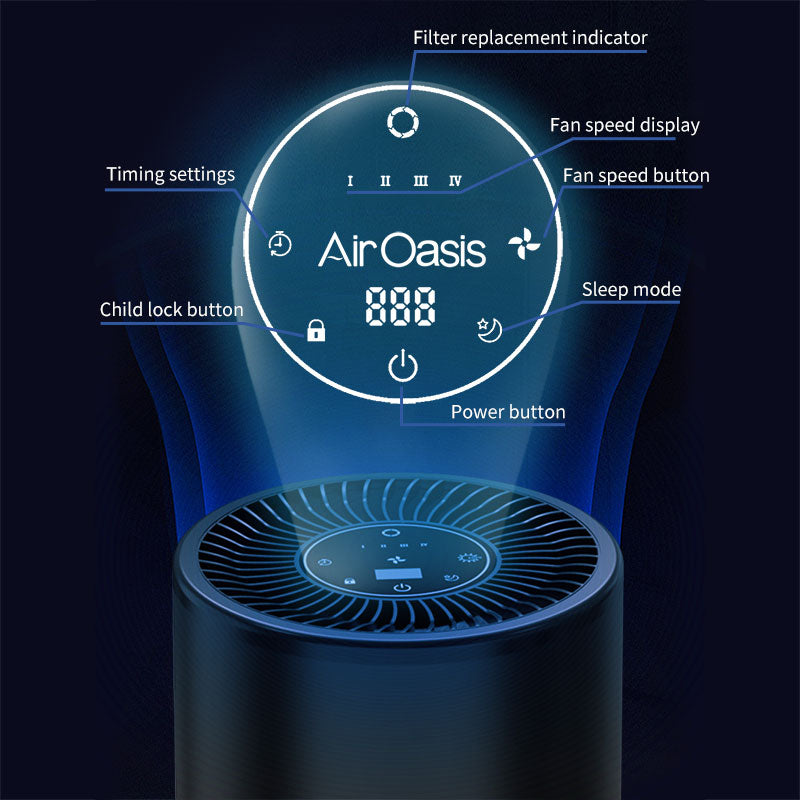
The iAdaptAir system captures 99% of airborne allergens that drain your energy through constant immune system activation. HEPA filtration removes the particles before you inhale them. Your body can rest instead of fighting perceived threats hour after hour. Better sleep follows when your airways aren't inflamed and congested from allergen exposure.
Stop accepting exhaustion as an inevitable part of having allergies. Clean air reduces the allergen load, triggering your immune system. Less inflammation means more energy. Better sleep means better daytime function. Shop Air Oasis today and reclaim the energy that allergies have been stealing from you.