When you visit your doctor for persistent asthma or breathing problems, they'll likely ask about your medications, your exercise habits, and your stress levels. But there's a good chance they won't ask about the air you're breathing at home—even though you spend more than 80% of your life indoors. According to Dr. Sarath Raju, Assistant Professor of Medicine at Johns Hopkins University School of Medicine, this oversight represents a significant missed opportunity in treating chronic respiratory conditions.
The Indoor Air Quality Gap in Clinical Care
Most clinicians simply aren't considering poor home air exposure when treating persistent asthma or airway disease, and this oversight may be affecting patient outcomes. Speaking at the American College of Chest Physicians Annual Meeting in Chicago, Dr. Raju emphasized that indoor air quality remains an understated subject in the growing field of environment-based medicine—despite being highly modifiable for individual patients.
The frustrating reality is that indoor air quality could foster clinical breakthroughs for patients with chronic conditions like asthma and chronic obstructive pulmonary disease. Yet the conversation rarely happens in exam rooms across the country. Patients struggling with uncontrolled symptoms may be prescribed new medications or higher doses when the real culprit might be cooking practices, inadequate ventilation, or environmental exposures right in their own homes.
When Indoor Air Should Enter the Conversation
Dr. Raju highlighted specific moments in clinical practice when indoor air quality questioning becomes particularly important—especially when patients report persistently uncontrolled asthma. Many patients actually feel worse inside their homes than in different environments, a telltale sign that something in their living space is triggering or worsening their symptoms.
The typical clinical approach focuses on pharmaceutical interventions: what new medicines can be added to change risk factors and modify disease. While medication remains important, Dr. Raju advocates for a more comprehensive approach that includes specific environmental factors that can be mitigated. The home environment offers numerous intervention points, from smoking inside the home to allergen exposure to different cooking practices.
Understanding Modifiable Indoor Exposures
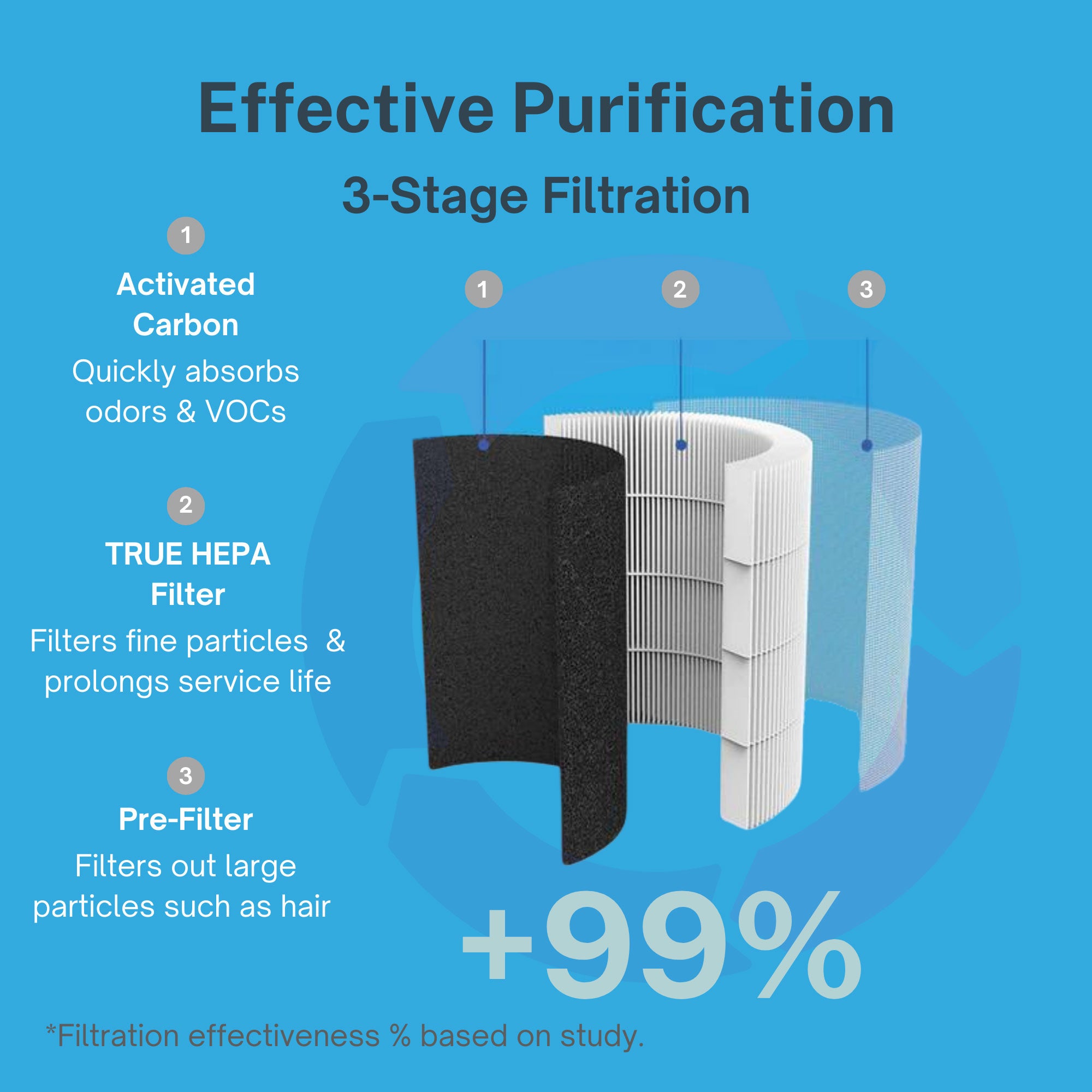
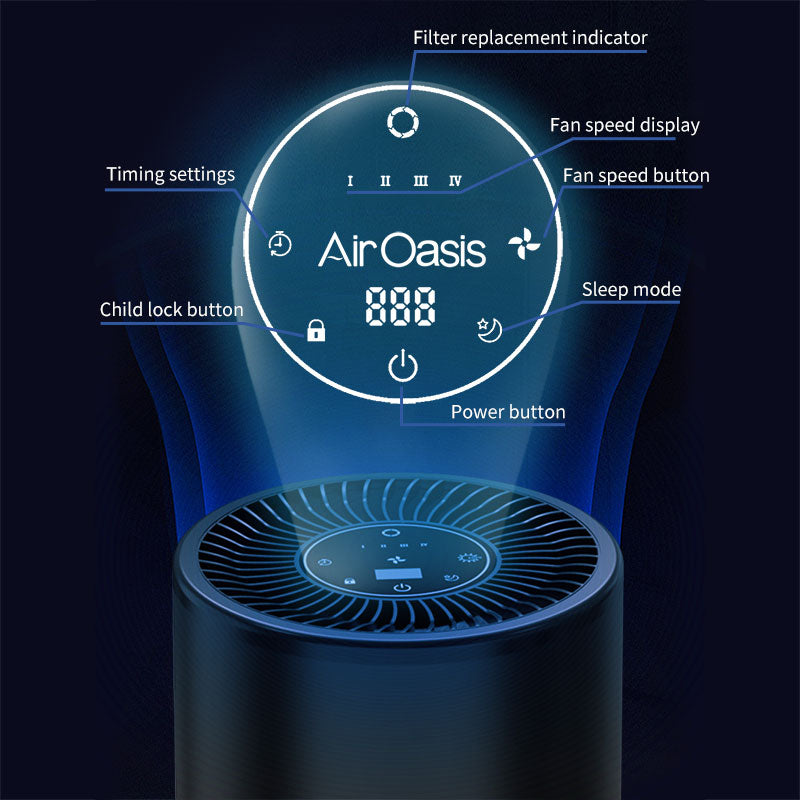
One significant concern involves cooking gas ovens, particularly in low-income communities where resources for mitigation may be limited. Different ventilation approaches and air filtration systems—including those with carbon filters—can reduce exposures, but implementation requires thinking creatively about what's feasible for each household.
Dr. Raju acknowledges that the medical community is still determining the best interventions to modify home environments, making this an important area for growth and future research. The challenge lies in identifying exposures that pose greater risk for someone with asthma and then proposing solutions that patients can actually implement in their daily lives.
Policy-level incentives and knowledge-based approaches both play roles in helping people understand these exposures and take action. For families with limited resources, the conversation must extend beyond expensive whole-home ventilation systems to include practical, affordable options that still make meaningful differences in air quality.
The Climate Connection
The conversation around indoor air quality intervention extends beyond immediate environmental factors. Climate change will inevitably force greater consideration of air quality-related prescriptions and treatment approaches, especially for pulmonary and allergic diseases. There's an important interaction between temperature and the indoor environment itself, and these two factors together can worsen respiratory symptoms and increase risk for respiratory viruses and other diseases.
As extreme weather events become more common and outdoor air quality fluctuates with increasing severity, the home becomes even more critical as a refuge. Creating cleaner indoor environments isn't just about comfort—it's about establishing a health-supporting sanctuary that can buffer against external environmental challenges.
Moving Toward Better Outcomes
The gap between what we know about indoor air quality and what gets discussed in clinical settings represents a real opportunity for improved patient outcomes. When clinicians begin routinely asking about home environments and patients become more aware of modifiable exposures, treatment plans can become more comprehensive and effective.
For patients dealing with persistent respiratory symptoms despite medication compliance, examining the home environment should be standard practice rather than an afterthought. The air you breathe in your living space matters just as much as the prescriptions in your medicine cabinet—perhaps even more so, given how many hours each day you spend breathing it.
Creating Your Health-Supporting Home Environment
While the medical community continues researching optimal interventions for indoor air quality, individuals don't have to wait for definitive answers to start making changes. Understanding that your home environment plays a crucial role in respiratory health empowers you to take action now, creating a living space that supports rather than undermines your wellbeing.
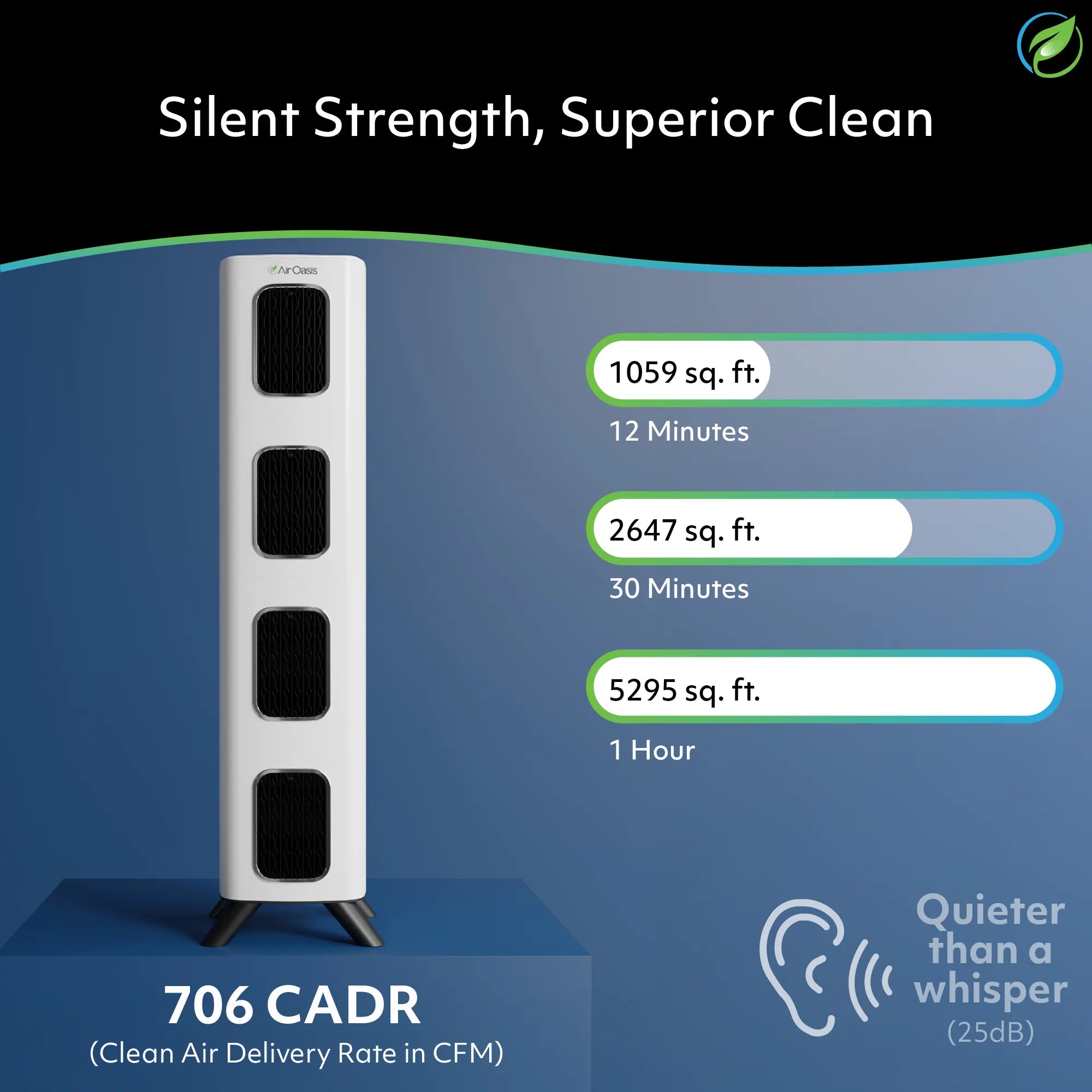
If you're ready to take control of your indoor air quality and support your respiratory health, advanced air purification technology offers a practical solution. Shop Air Oasis today and create the clean-air sanctuary your lungs deserve.