The cough never really stops. Morning brings up thick mucus. Climbing stairs leaves you wheezing. Cold air triggers immediate chest tightness. And when the air quality index climbs, everything gets worse.
Chronic bronchitis means living with perpetually inflamed airways. The bronchial tubes that carry air to your lungs stay swollen and produce excess mucus. You cough constantly, trying to clear passages that just keep filling up. And air pollution makes every symptom more severe.
Understanding how air quality affects chronic bronchitis could help you manage symptoms more effectively and prevent the exacerbations that lead to emergency room visits.
What Chronic Bronchitis Does to Your Airways
Chronic bronchitis involves long-term inflammation of the bronchial tubes. These airways connect your windpipe to the smaller passages deep in your lungs. Healthy bronchial tubes have smooth inner linings that move air efficiently. Chronic bronchitis transforms them into inflamed, mucus-producing tissues that obstruct airflow.
The inflammation thickens airway walls. Mucus-producing cells multiply and become overactive. Cilia, the tiny hair-like structures that normally sweep mucus out of airways, become damaged or destroyed. The result is excess mucus that accumulates faster than your body can clear it.
Doctors diagnose chronic bronchitis when you have a productive cough lasting at least three months for two consecutive years. Smoking causes most cases. But air pollution plays a significant role in both disease development and symptom severity.
Your already inflamed airways can't handle additional irritants. When air pollution levels rise, your compromised respiratory system faces burdens it can't manage. Symptoms intensify. Breathing becomes harder. The risk of serious complications increases.
How Air Pollution Triggers Bronchitis Symptoms
Particulate matter represents the most dangerous pollutant for people with chronic bronchitis. PM2.5 particles measuring 2.5 micrometers or smaller penetrate deep into your respiratory system. These microscopic fragments reach the inflamed bronchial tubes and trigger cascading responses.
The particles activate immune cells in airway walls. White blood cells release inflammatory chemicals. Blood flow to the area increases. Mucus production ramps up. The airways that were already narrowed by chronic inflammation constrict further.
Your morning cough becomes more persistent. The mucus you're bringing up increases in volume and thickness. Wheezing intensifies because air struggles to move through constricted, mucus-filled passages. Shortness of breath worsens with even minimal exertion.
Ground-level ozone creates additional problems. This gas forms when sunlight reacts with pollutants from vehicles and industrial sources. Ozone directly damages the delicate lining of airways. It increases mucus production and makes the cilia that remain functional work less efficiently.
Nitrogen dioxide from vehicle exhaust and gas appliances irritates inflamed tissues. Sulfur dioxide triggers bronchospasm, causing airways to constrict suddenly. Each pollutant adds to your symptom burden. The combined effect during high pollution episodes can push stable chronic bronchitis into acute exacerbation.
The Exacerbation Cycle
An acute exacerbation means a sudden worsening of symptoms beyond your baseline. Your cough becomes more severe. Mucus production increases dramatically and may change color. Breathing difficulty intensifies. You might develop fever or feel exhausted.
These episodes often require medical intervention. Antibiotics treat bacterial infections that commonly accompany exacerbations. Steroids reduce airway inflammation. Bronchodilators help open constricted airways. Some people need hospitalization for oxygen support or more intensive treatment.
Air pollution commonly triggers these dangerous episodes. Studies show clear correlations between elevated PM2.5 levels and increased bronchitis hospitalizations. Even short-term exposure to high pollution can destabilize someone with well-managed chronic bronchitis.
The mechanism involves overwhelming your airways' limited defenses. Your damaged cilia can't clear the increased mucus load. Bacteria colonize the accumulated mucus, causing infections. The infection triggers more inflammation. More inflammation produces more mucus. The cycle spirals into crisis.
Wildfire smoke creates particularly hazardous conditions. The PM2.5 concentrations during major smoke events reach levels that would challenge even healthy lungs. For someone with chronic bronchitis, these conditions become life-threatening. Emergency departments see dramatic spikes in bronchitis admissions during wildfire seasons.
Indoor Air Quality Presents Hidden Dangers
You might assume staying indoors protects you from outdoor pollution. But indoor air often contains higher pollutant concentrations than outdoor air, especially without active filtration.
Cooking generates significant particulate matter. Frying foods releases grease particles and combustion byproducts. Gas stoves emit nitrogen dioxide that directly irritates your inflamed airways. Your kitchen air can reach pollution levels that would trigger outdoor air quality warnings.
Cleaning products add volatile organic compounds to indoor air. These chemicals irritate respiratory tissues and can trigger bronchospasm. Common household cleaners, air fresheners, and disinfectants all contribute to indoor pollution that worsens bronchitis symptoms.
Dust accumulation provides another source of airway irritation. Dust mites produce allergenic proteins. Pet dander contains similar irritants. Mold spores trigger inflammatory responses. Without filtration, these particles circulate continuously through your living space.
Secondhand smoke represents an especially severe threat. Even if you've quit smoking, exposure to others' tobacco smoke worsens chronic bronchitis. The particles and gases in smoke trigger immediate symptom flares and accelerate long-term disease progression.
Creating Your Clean Air Sanctuary
You can't control outdoor air quality. But you can create a clean air environment inside your home where you spend most of your time. Medical-grade air purification provides the most effective protection available.
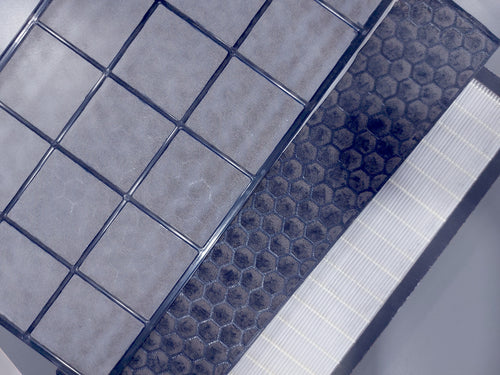
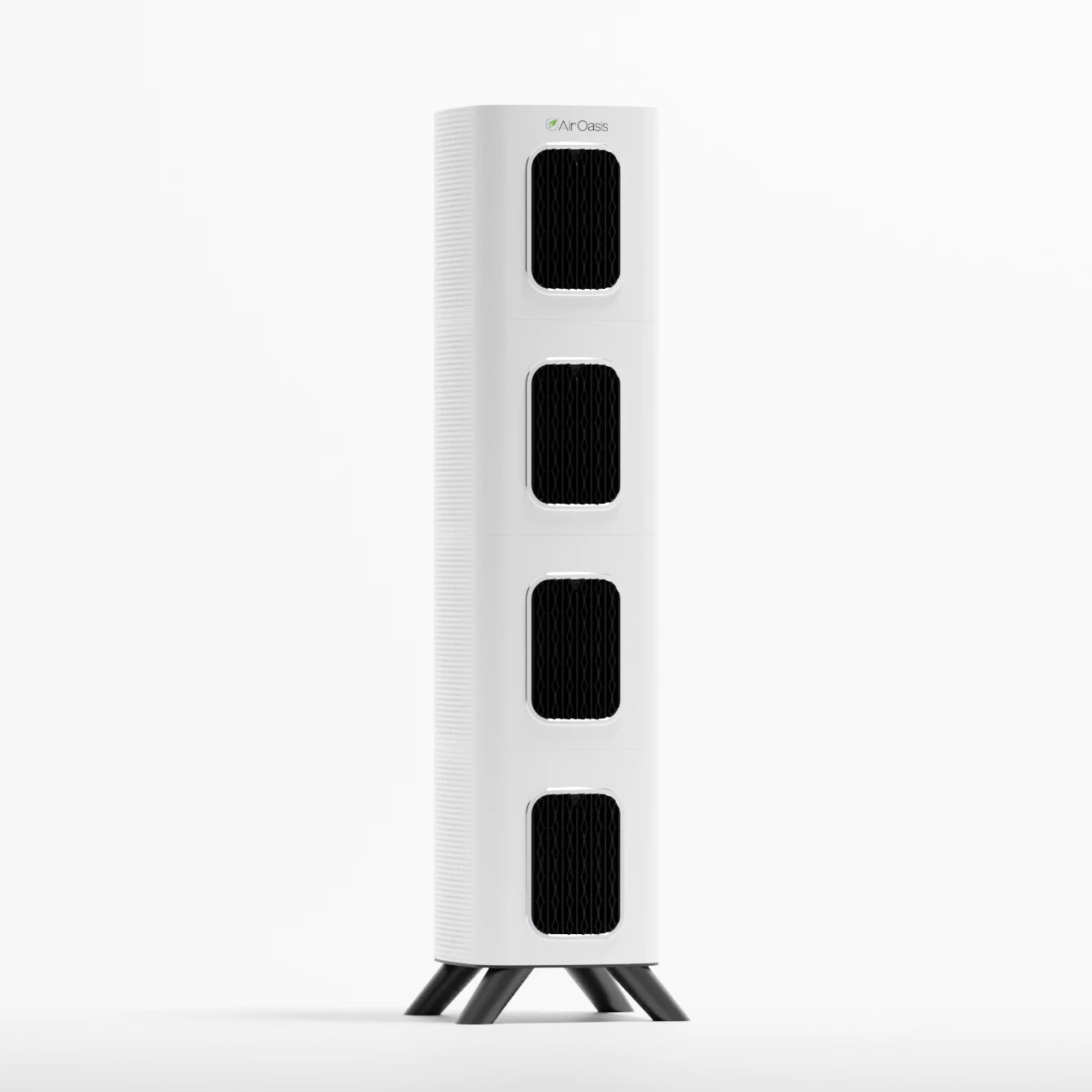
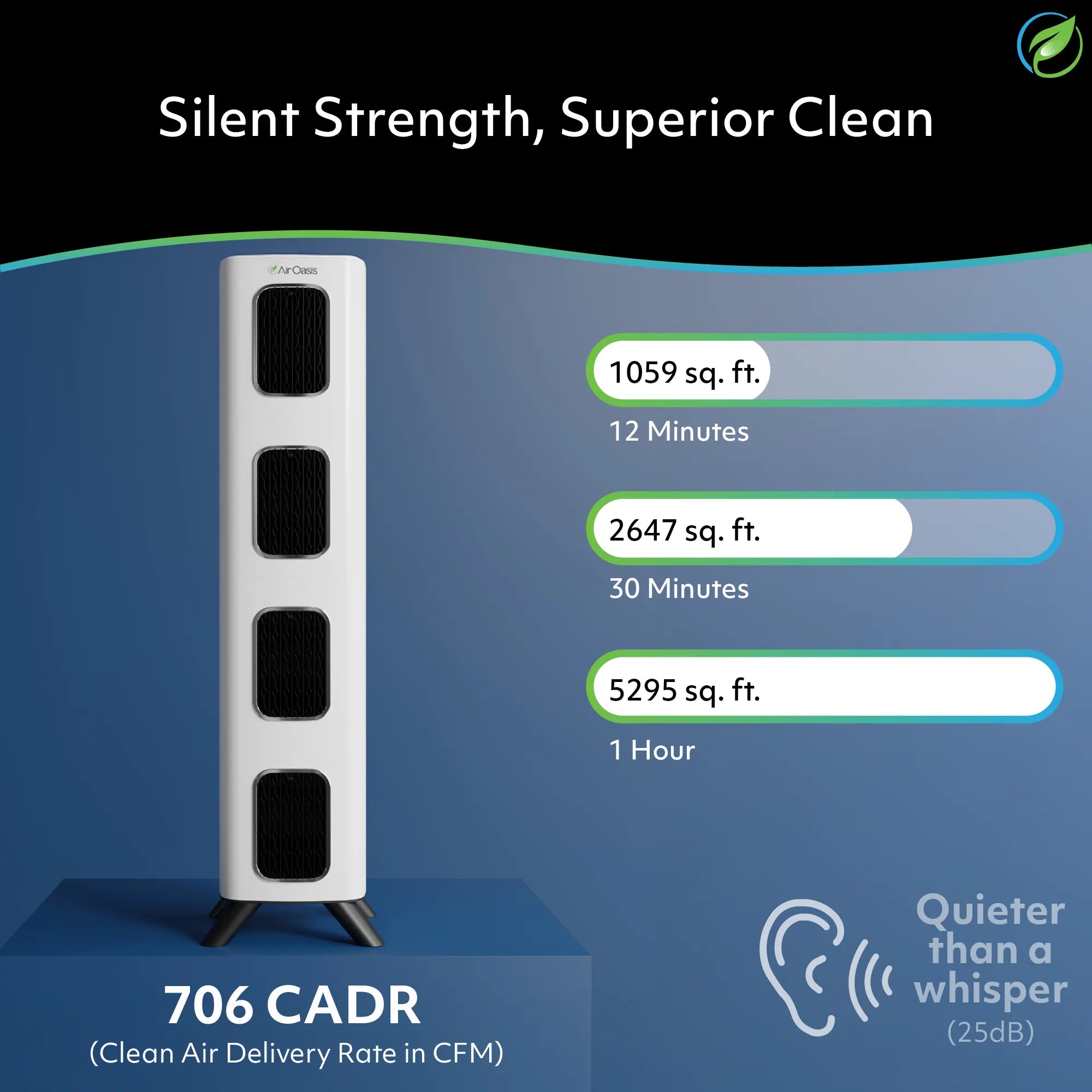
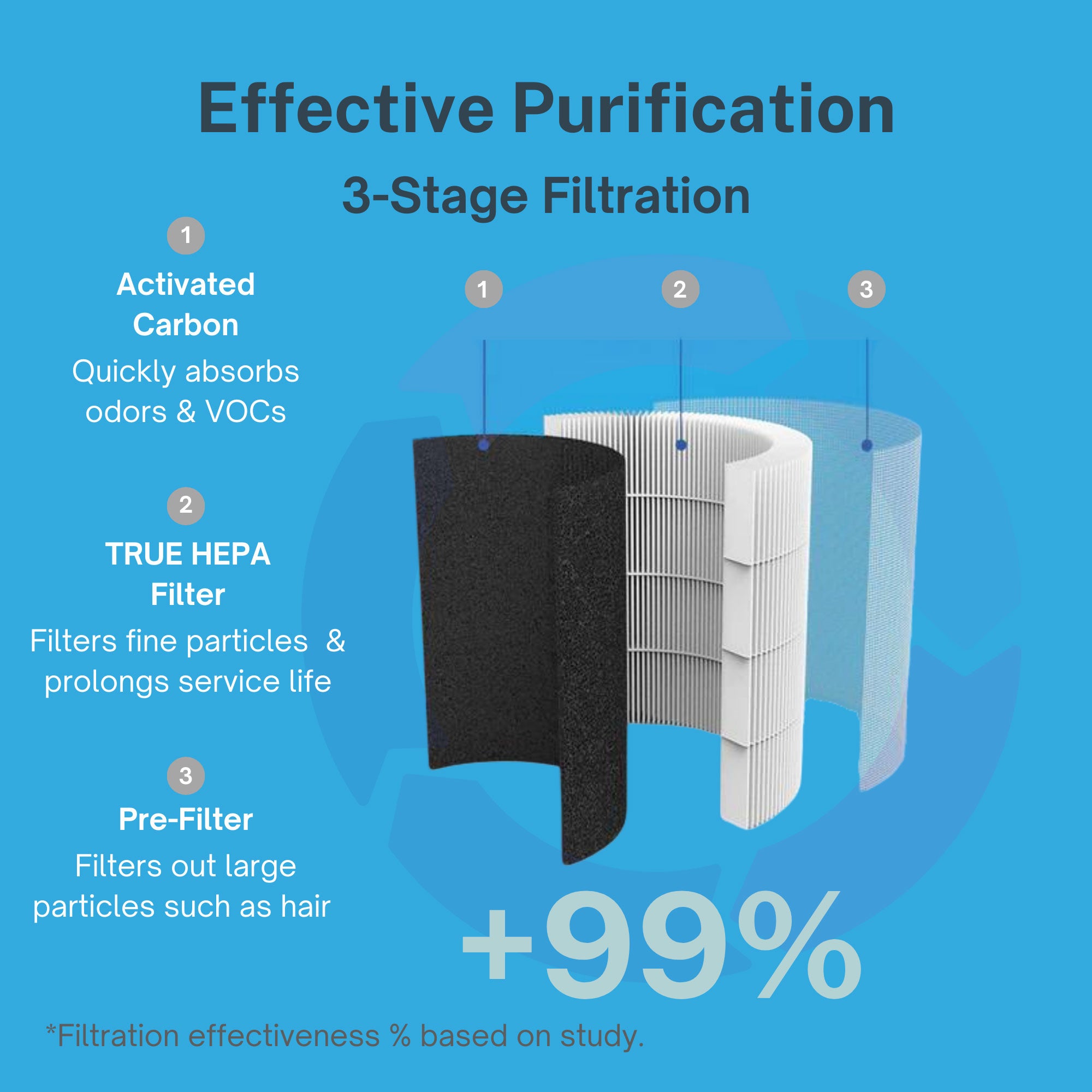
HEPA filtration removes 99.97 percent of particles as small as 0.3 micrometers. That includes PM2.5 from cooking, outdoor infiltration, dust, and other sources. The iAdaptAir system processes room air continuously, capturing particles before they reach your inflamed bronchial tubes.
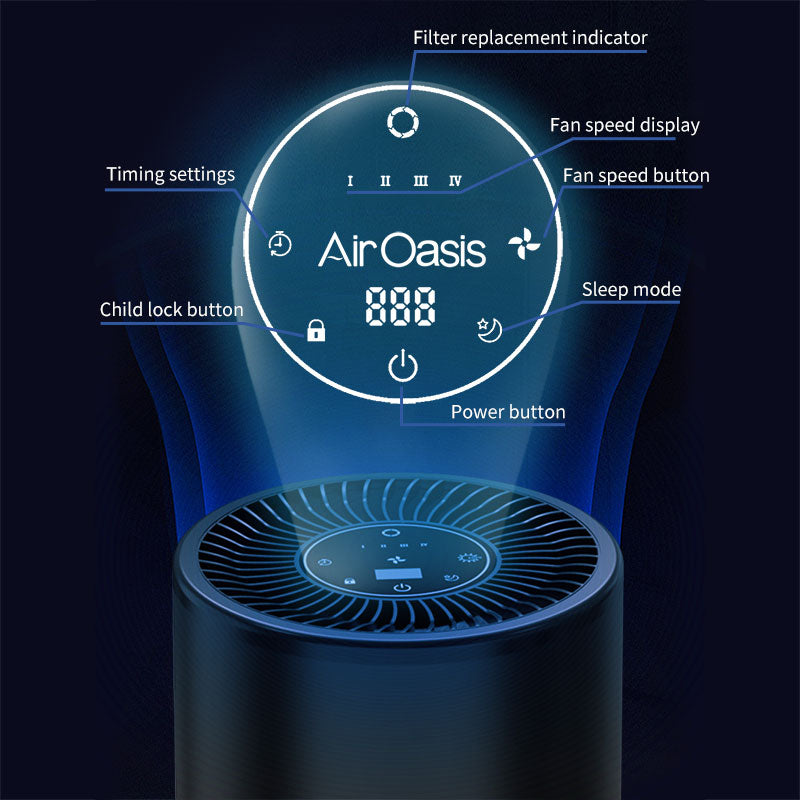
Smart sensors monitor air quality in real time. When particulate levels rise, fan speeds increase automatically to match the challenge. During cooking or when outdoor pollution infiltrates through ventilation systems, filtration intensifies. You get protection that adapts to actual conditions rather than running at fixed settings.
UV-C technology adds crucial pathogen control. People with chronic bronchitis face increased infection risk because damaged airways can't clear bacteria effectively. UV-C light neutralizes these biological threats before they can colonize the excess mucus in your airways.
Activated carbon filtration removes gaseous pollutants including volatile organic compounds and nitrogen dioxide. This comprehensive approach addresses the full spectrum of indoor air quality threats, not just particulate matter. Fewer irritants mean fewer symptom flares and reduced exacerbation risk.
Managing Bronchitis in a Polluted World
Air purification provides essential protection. But chronic bronchitis management requires multiple strategies working together. Monitor air quality forecasts daily. On high pollution days, stay indoors with your air purifier running. Postpone outdoor activities until conditions improve.
Keep rescue medications readily available. Poor air quality can trigger sudden symptom worsening even with good baseline control. Having bronchodilators within reach allows immediate response to breathing difficulties.
Follow your treatment plan consistently. This includes prescribed medications, pulmonary rehabilitation if recommended, and regular medical follow-ups. Air purification enhances these standard treatments but doesn't replace them.
Avoid indoor pollution sources when possible. Use exhaust fans while cooking. Choose fragrance-free, low-VOC cleaning products. Don't burn candles or use air fresheners that add particles and chemicals to indoor air. Every reduction in irritant exposure helps protect your inflamed airways.
Breathe Easier Starting Today
Chronic bronchitis already makes breathing difficult. Don't let indoor air pollution make symptoms worse. You deserve air that supports your respiratory health rather than triggering constant inflammation.
The iAdaptAir system delivers medical-grade filtration designed to remove the pollutants that worsen chronic bronchitis. HEPA technology captures PM2.5 particles. UV-C neutralizes pathogens. Smart sensors ensure continuous protection adapted to your home's air quality.
Give your inflamed airways the cleanest possible air to breathe. Shop Air Oasis today and create the healthy indoor environment your lungs desperately need.