Chronic Inflammatory Response Syndrome affects multiple body systems through complex biochemical pathways triggered by biotoxin exposure. Among the many health concerns associated with CIRS, research has identified specific blood coagulation abnormalities that increase the risk of both excessive clotting and unexplained bleeding. Understanding these clotting disorders helps patients and healthcare providers recognize warning signs and implement appropriate monitoring strategies.
The Connection Between CIRS and Blood Coagulation
Research into CIRS has revealed that the inflammatory cascade triggered by biotoxin exposure doesn't limit itself to respiratory symptoms or cognitive issues. The condition impairs blood clotting through several distinct mechanisms. When inflammatory elements persist in the bloodstream, they interact with various components of the coagulation system, creating conditions where both excessive clotting and unexpected bleeding can occur.
The biotoxin pathway identified by researchers involves multiple inflammatory markers that directly impact blood vessel integrity and clotting factors. Two specific abnormalities appear with notable frequency in CIRS patients: acquired von Willebrand disease and elevated anticardiolipin antibodies. Both conditions significantly alter normal hemostasis and create potential health risks that require medical attention.
Acquired von Willebrand Disease in CIRS
Von Willebrand disease represents one of the most common genetic clotting disorders, characterized by increased bleeding tendencies. However, CIRS patients can develop what researchers call "acquired" von Willebrand disease, in which normal clotting factors are disrupted by inflammatory processes rather than by genetic inheritance.
Research has documented that when CIRS creates a hemostatic challenge through autoimmune and connective tissue dysregulation, acquired von Willebrand disease may manifest, causing unexpected bleeding that proves difficult to stop. Clinical findings in CIRS patients include frequent nosebleeds, easy bruising, bleeding from mucosal surfaces, and hemoptysis.
The mechanism behind this acquired condition involves multiple factors. Research has proposed that CIRS may trigger the development of autoantibodies, selective absorption of high molecular weight von Willebrand factor multimers, mechanical destruction of von Willebrand factor under high shear stress, and increased proteolysis. Laboratory analysis in affected patients shows low levels of Factor VIII, reduced ristocetin-associated cofactor, and decreased multimers of von Willebrand antigen.
The inflammatory marker C4a, which elevates significantly in CIRS patients exposed to water-damaged buildings, appears to play a role in this coagulation disruption. Research indicates that C4a can interact with von Willebrand factor polymerization, leading to bleeding from mucosal surfaces. When patients report frequent nosebleeds, easy bruising, or bleeding tendencies, acquired von Willebrand disease warrants investigation as the blood coagulation system represents another enzyme-triggered cascade affected by CIRS.
Anticardiolipin Antibodies and Thrombosis Risk
While acquired von Willebrand disease creates bleeding risks, CIRS patients also face the opposite problem through elevated anticardiolipin antibodies. These autoantibodies target the cardiolipin component of cell membranes, increasing the risk of both blood clotting and abnormal bleeding.
Anticardiolipin antibodies commonly appear in collagen vascular diseases such as lupus and scleroderma. In CIRS patients, these antibodies create multiple complications, including increased risk for miscarriage, blood clots in veins or arteries, low platelet counts through autoimmune thrombocytopenia, stroke, transient ischemic attacks, formation of clots on heart valves, pulmonary emboli, and pulmonary hypertension.
Livedo reticularis, a mottled purplish discoloration of the skin in a net-like pattern, represents a common presenting sign of elevated anticardiolipin antibodies. This visible symptom can alert both patients and healthcare providers to investigate further for coagulation abnormalities. The presence of these antibodies indicates that CIRS has triggered autoimmune processes affecting the cardiovascular system beyond the more commonly recognized respiratory and neurological impacts.
Additional Clotting Risk Factors in CIRS
Beyond von Willebrand abnormalities and anticardiolipin antibodies, CIRS affects other components of the coagulation system. Research has identified elevated plasminogen activator inhibitor-1 in CIRS patients. This serine protease inhibitor, secreted by blood vessel endothelial layers and adipose tissue, inhibits fibrinolysis, increases clotting, and creates an increased risk for thrombosis.
When plasminogen activator inhibitor-1 combines with Matrix Metalloproteinase-9, another marker frequently elevated in CIRS, it facilitates oxidized LDL movement through blood vessel walls. This brings inflammatory elements into the subintimal space, potentially causing connective tissue fibrosis and contributing to atherosclerosis development. The combination of these factors suggests CIRS patients may face increased cardiovascular disease risk beyond immediate clotting concerns.
Clinical Implications and Monitoring
The presence of coagulation abnormalities in CIRS patients requires careful clinical assessment and ongoing monitoring. Healthcare providers evaluating CIRS patients should consider testing for acquired von Willebrand disease when patients report epistaxis or hemoptysis. The von Willebrand profile includes Factor VIII levels, ristocetin associated cofactor, and von Willebrand antigen multimers.
Anticardiolipin antibodies testing includes IgA, IgG, and IgM measurements. Reference ranges indicate negative results as IgA less than 11 APL units, IgG less than 14 GPL units, and IgM less than 12 MPL units. Elevations beyond these thresholds signal increased clotting risk and warrant preventive strategies.
Research indicates these coagulation abnormalities often reverse when the underlying CIRS receives appropriate treatment. Studies have shown that addressing biotoxin exposure, reducing inflammatory markers, and following systematic treatment protocols can restore normal hemostasis in most cases. This reversibility suggests the coagulation problems stem from active inflammatory processes rather than permanent damage to clotting factors.
Treatment Approaches for Coagulation Issues
Clinical research has identified specific interventions that address coagulation abnormalities in CIRS patients. For acquired von Willebrand disease, the use of DDAVP can rapidly reduce hemorrhage by enhancing the polymerization of von Willebrand multimers and making platelets stickier. This intervention provides quick management of acute bleeding episodes while the underlying CIRS treatment progresses.
The comprehensive CIRS treatment protocol developed through clinical research aims to normalize all inflammatory markers, which includes restoring proper coagulation function. As treatment reduces biotoxin load and corrects the inflammatory cascade, coagulation abnormalities typically resolve alongside other CIRS symptoms. Regular monitoring throughout treatment ensures coagulation factors return to normal ranges and bleeding or clotting risks diminish.
Protecting Your Health from CIRS Complications
The blood coagulation abnormalities associated with CIRS represent serious health concerns requiring medical attention and ongoing monitoring. Both excessive bleeding tendencies and increased clotting risk can develop through the inflammatory processes triggered by biotoxin exposure. Recognition of symptoms like frequent nosebleeds, easy bruising, or livedo reticularis should prompt evaluation for these coagulation disorders.
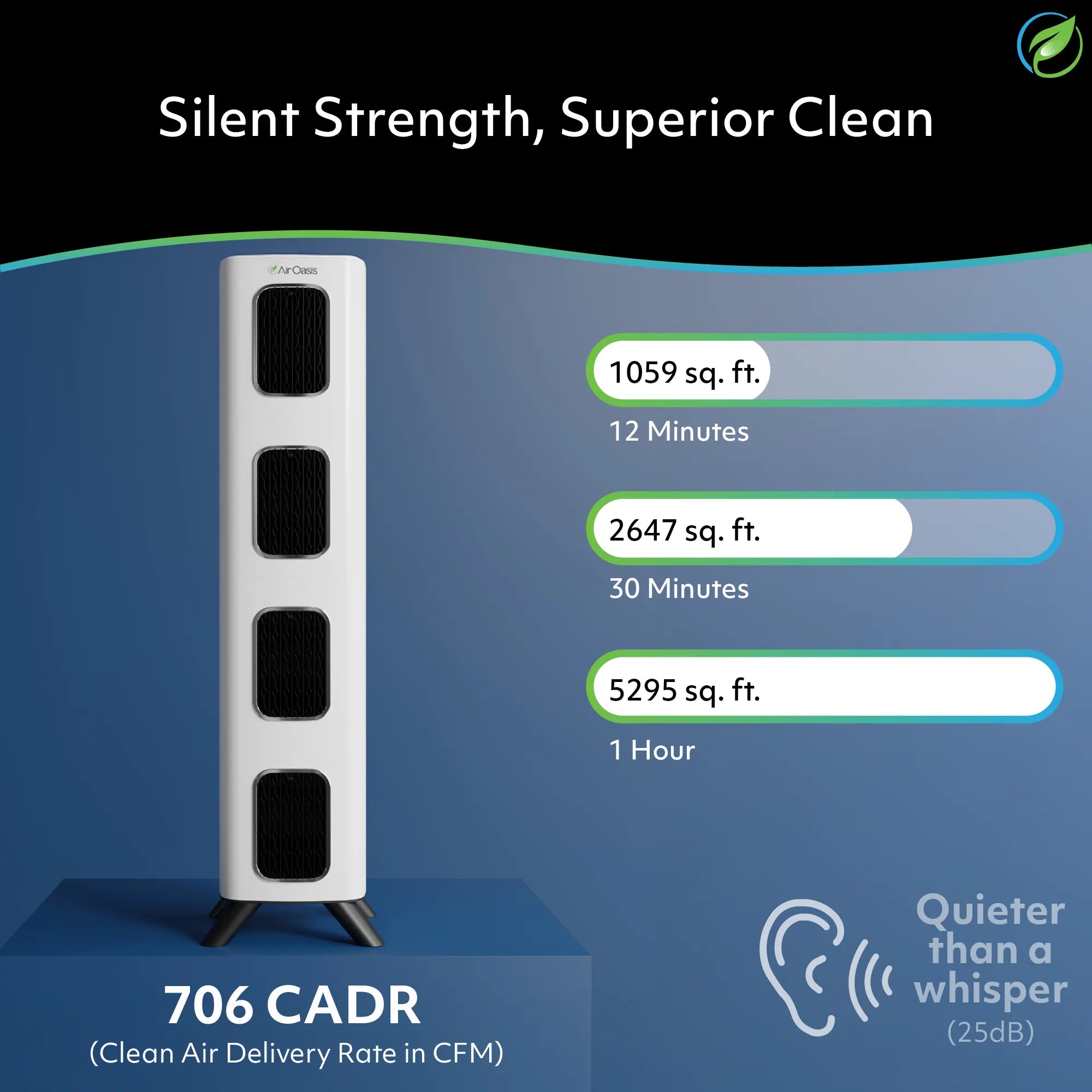
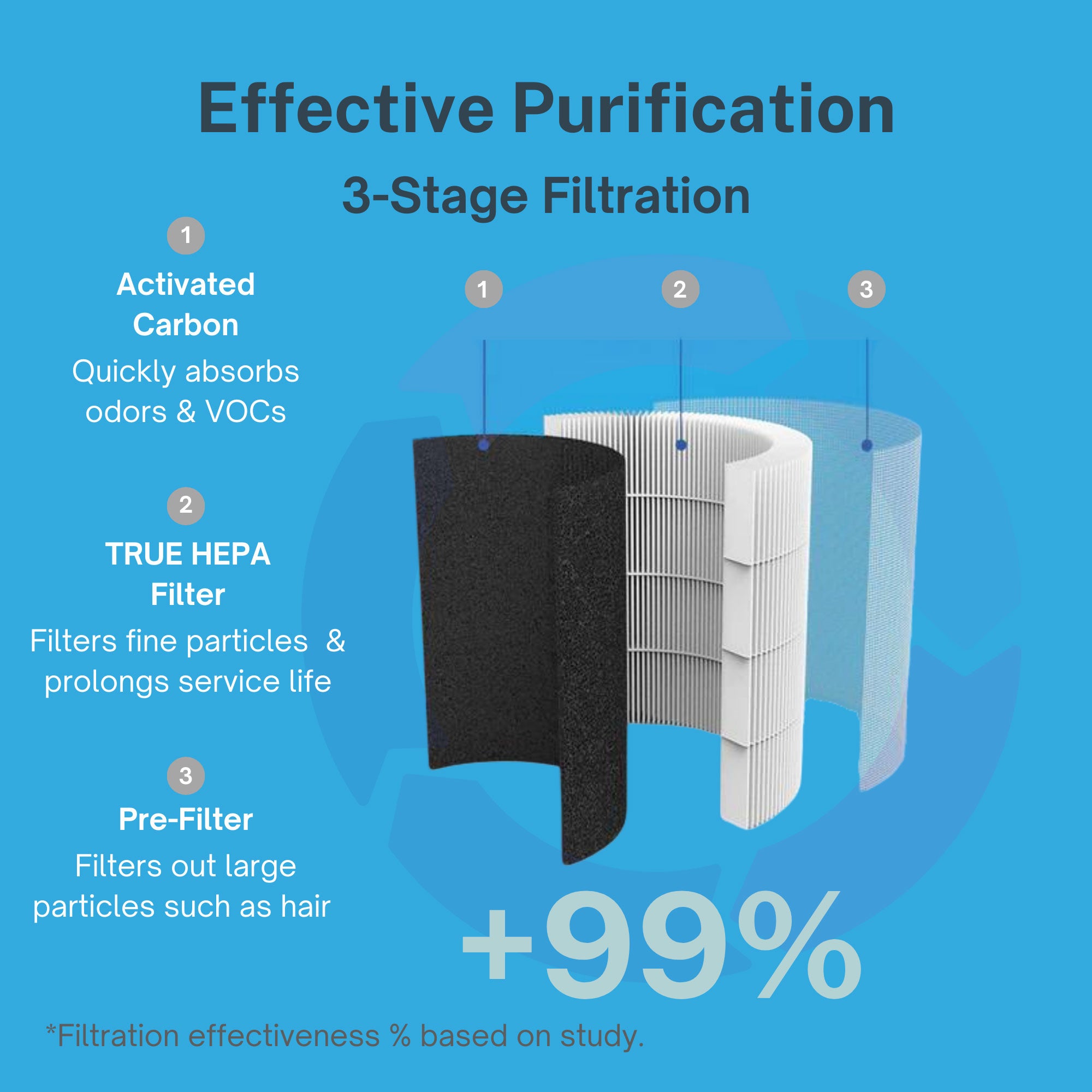
Addressing CIRS comprehensively requires more than managing individual symptoms—it demands removal from biotoxin exposure and systematic correction of the inflammatory cascade affecting multiple body systems, including the blood coagulation system. Clean indoor air, free from water-damage contaminants, provides the foundation for preventing CIRS development and its associated complications. If you're concerned about biotoxin exposure in your home or workplace, shop Air Oasis today and create an environment that supports rather than compromises your cardiovascular health.