Your rheumatoid arthritis symptoms worsen after moving into your new apartment. Your multiple sclerosis flares more frequently since water damage appeared in your basement. Could mold exposure actually be triggering or worsening your autoimmune condition?
The Autoimmune-Mold Connection Remains Controversial
The relationship between mold exposure and autoimmune disease development sparks heated debate in medical communities. Some practitioners observe clear connections between mold exposure and autoimmune symptoms in their patients. Critics argue insufficient evidence exists to prove mold directly causes autoimmune diseases.
Current scientific consensus suggests mold and mycotoxins probably don't directly cause autoimmune diseases in previously healthy individuals. However, emerging evidence indicates something more nuanced. Mold exposure appears particularly problematic for people with existing immune system dysregulation. In these vulnerable individuals, mycotoxins may trigger disease onset or dramatically worsen existing autoimmune conditions.
This distinction matters enormously. If you already have immune system imbalances or genetic susceptibilities, mold exposure poses different risks than it does for people with normal immune function. Understanding this difference helps explain why some people develop severe problems from mold while others remain unaffected.
How Mycotoxins Affect Immune Function
Mycotoxins represent toxic secondary metabolites produced by molds. These compounds cross into your bloodstream regardless of exposure route. Whether you inhale mold spores or ingest contaminated food, mycotoxins become systemically available throughout your body.
Once circulating, mycotoxins interfere with immune function through multiple mechanisms. They compromise barrier functions in your gut, lungs, and even blood-brain barrier. Weakened barriers allow inflammatory molecules and antigens to enter tissues that normally remain protected.
Mycotoxins also trigger excessive inflammatory responses. They activate inflammasomes, cellular complexes that drive inflammation production. This overactivation generates reactive oxygen species and inflammatory cytokines that damage tissues. The chronic inflammatory state created by mycotoxin exposure resembles the inflammation seen in autoimmune diseases.
Genetic susceptibility plays a critical role in these responses. Approximately 25% of people carry HLA-DR gene variants that prevent efficient mycotoxin clearance. These individuals experience prolonged mycotoxin exposure even after leaving contaminated environments. Their immune systems remain activated chronically, unable to properly eliminate the triggering substances.
Multiple Sclerosis and Neurological Autoimmunity
Research documents concerning connections between mold exposure and multiple sclerosis. Studies found elevated neural protein autoantibodies in people exposed to water-damaged buildings. These antibodies target proteins in brain and nervous system tissue including myelin basic protein, tau, and tubulin.
One study examined eight women with known mold exposure. All tested positive for IgG antibodies against multiple neuronal proteins. However, this research had limitations—mycotoxin measurements in blood or urine were missing. Other factors besides mold could potentially cause these antibody elevations.
Animal studies provide stronger evidence. Mice exposed to gliotoxin, a mycotoxin from Aspergillus molds, showed worsened experimental autoimmune encephalomyelitis. This animal model mimics multiple sclerosis. Gliotoxin exposure increased neuroinflammation and accelerated myelin destruction in affected mice.
The mechanism appears to involve direct mycotoxin effects on brain immune cells called microglia. These cells become overactivated, producing inflammatory molecules that damage surrounding neurons. The blood-brain barrier also becomes more permeable, allowing additional inflammatory substances to enter brain tissue.
Rheumatoid Arthritis Connections
Limited research examines mold's role in rheumatoid arthritis. One small 1980s study found RA patients showed stronger reactions to Aspergillus antigens than healthy controls. However, no recent human studies have investigated this relationship further.
Animal research provides more compelling evidence. Mice exposed to ochratoxin A and deoxynivalenol, two common mycotoxins, developed increased rheumatoid arthritis susceptibility and severity. The exposed mice showed elevated clinical scores for paw inflammation with tissue analysis revealing infiltrated white blood cells, joint tissue overgrowth, cartilage destruction, and bone erosion.
The mechanism involves enhanced activation of immune cells that produce inflammatory cytokines. These include IL-1β, IL-6, and TNF-α—the same inflammatory molecules targeted by expensive biologic drugs used to treat RA. Mycotoxin exposure appears to promote Th1 and Th17 immune cell differentiation, immune pathways known to drive autoimmune inflammation.
Inflammatory Bowel Disease Development
Emerging evidence suggests mycotoxins may trigger inflammatory bowel disease onset in susceptible individuals. One case report described a 25-year-old man with refractory ulcerative colitis who tested positive for trichothecene mycotoxins. After eliminating mold exposure, his pancreatitis symptoms resolved, though colitis required continued medical treatment.
Animal studies provide stronger support. Rats exposed to deoxynivalenol showed increased colon damage and inflammation. The mycotoxin worsened colitis symptoms in disease models. Exposed animals developed morphological intestinal changes and elevated inflammatory markers including myeloperoxidase and IL-1β.
Mycotoxins may affect gut bacteria composition, creating dysbiosis. This imbalance in intestinal microorganisms represents a known risk factor for IBD development. The combination of barrier damage, dysbiosis, and inflammatory activation creates conditions favorable for chronic intestinal inflammation.
The Exacerbation Factor
The most important takeaway involves understanding mold's role as an exacerbating factor rather than a primary cause. In people with pre-existing immune dysregulation, mold exposure acts like gasoline on smoldering fire. The underlying immune imbalance already exists. Mycotoxins intensify and accelerate disease progression.
This explains why some people develop severe autoimmune symptoms from mold exposure while others show no effects. Genetic susceptibility, existing immune dysfunction, and cumulative exposure duration all influence outcomes. The more vulnerable your immune system, the greater your risk.
For people with diagnosed autoimmune conditions, eliminating mold exposure becomes critical. Continued mycotoxin exposure perpetuates inflammation that drives disease activity. Removing this trigger allows immune systems to stabilize and potentially reduces disease severity.
Protecting Your Immune Health
Clean indoor air quality proves essential for anyone with autoimmune disease or immune dysregulation. Mold spores and mycotoxins in your home environment continuously challenge your immune system. Medical-grade air purification removes these triggers.
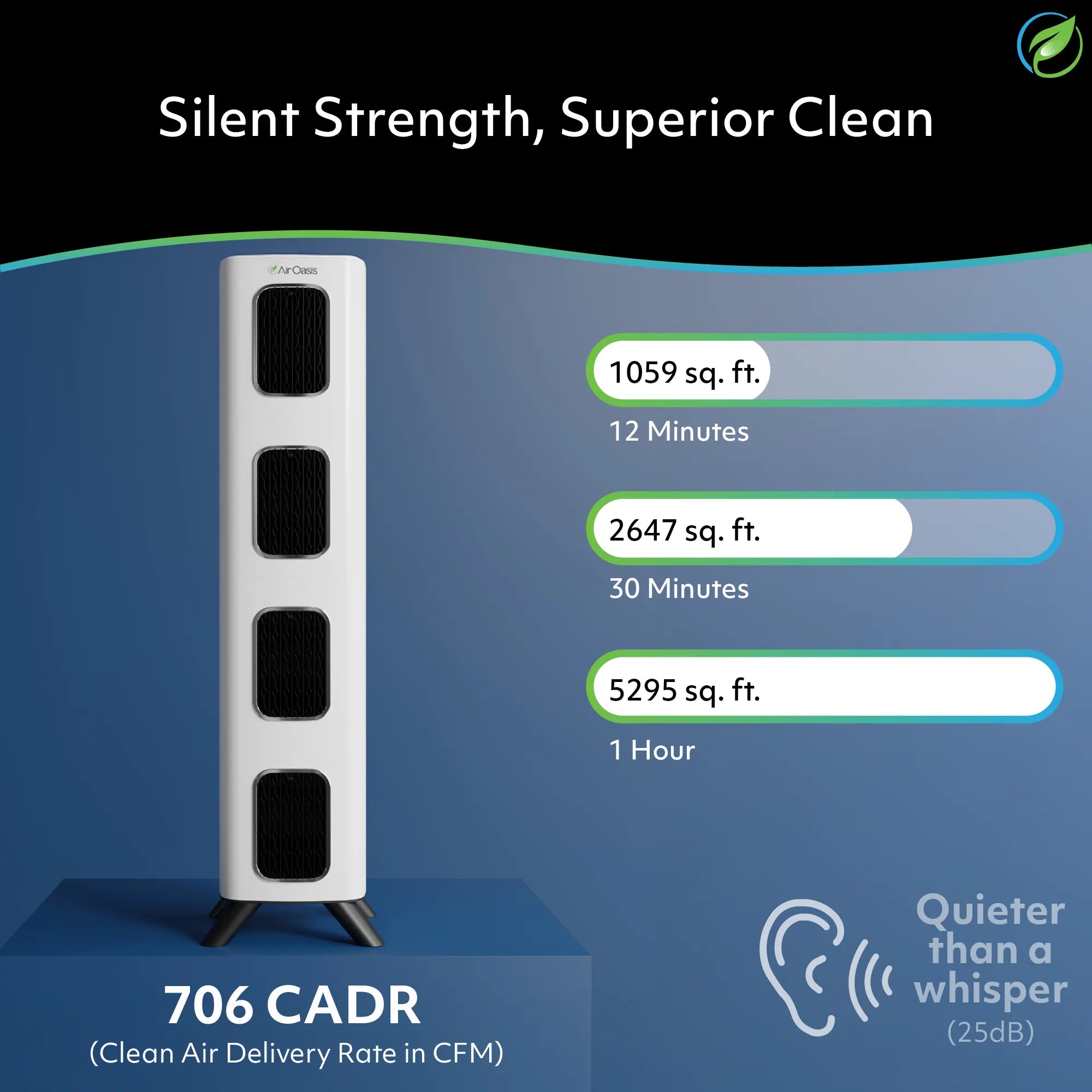
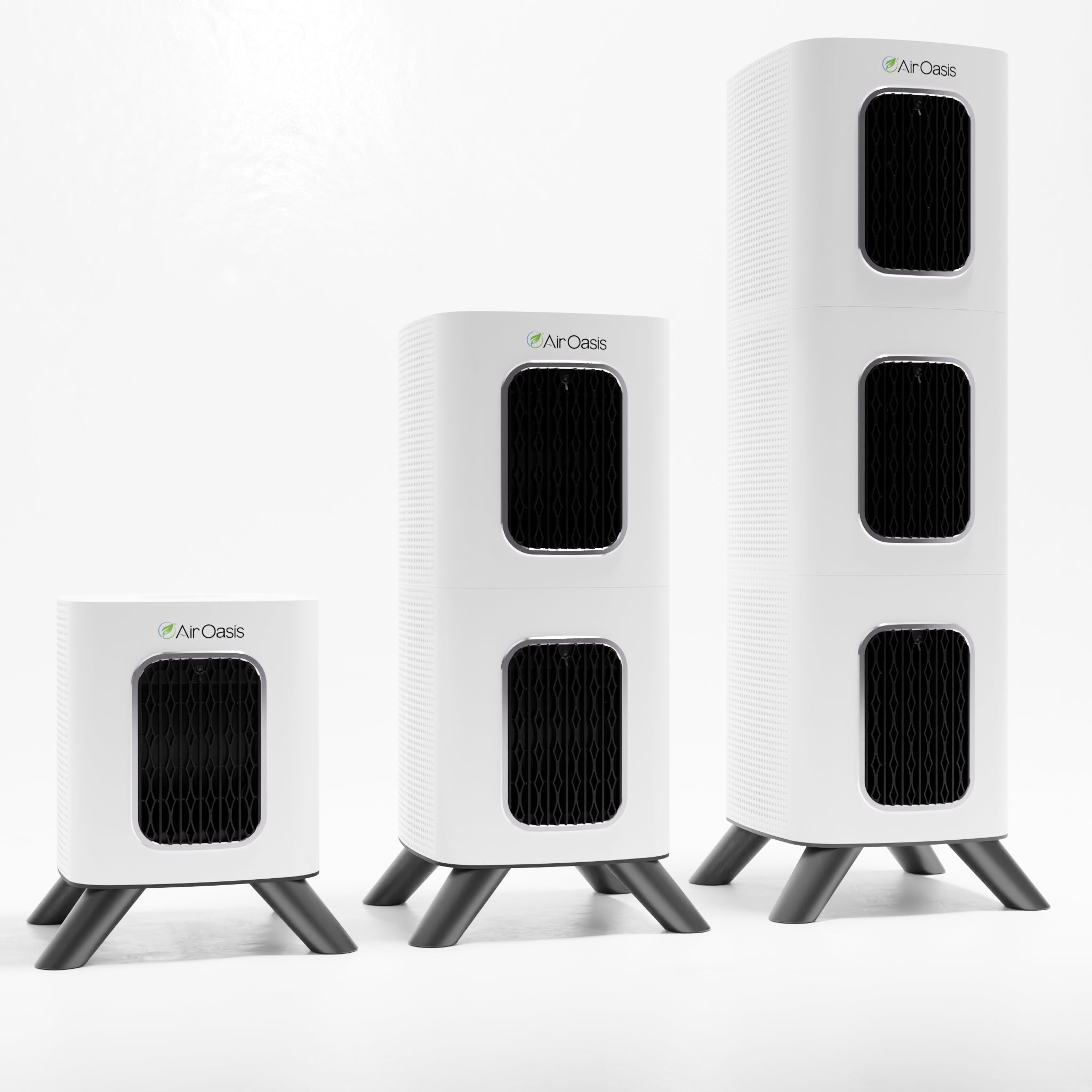
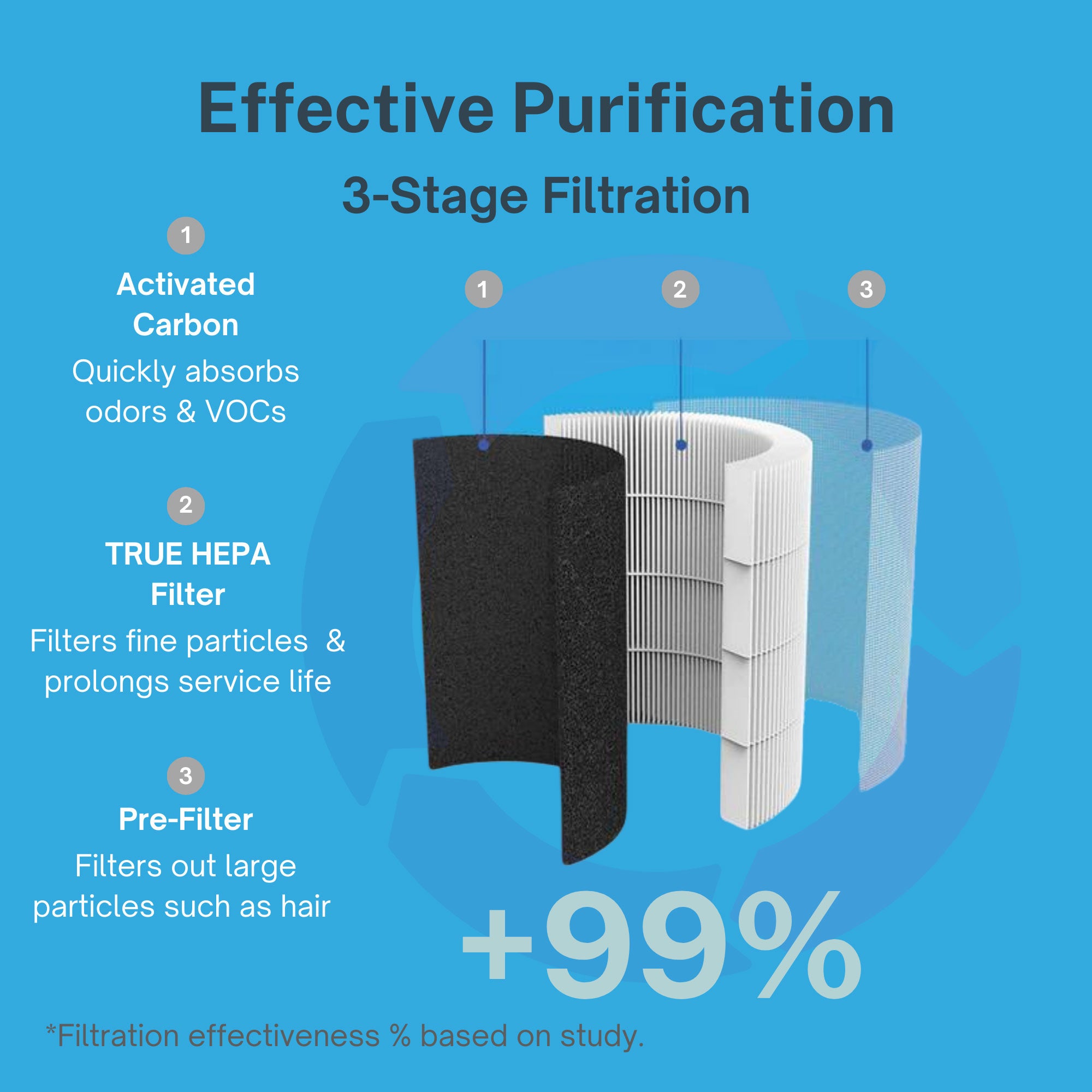
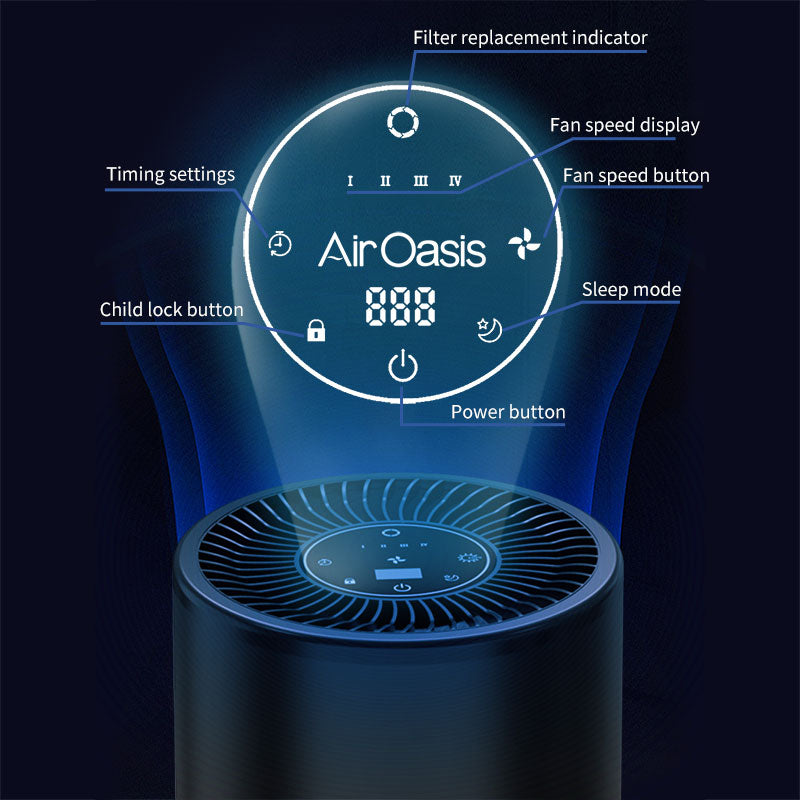
The iAdaptAir series provides comprehensive protection against mold-related immune challenges. HEPA filtration captures 99.97% of mold spores and fragments down to 0.3 microns. Activated carbon removes volatile organic compounds from mold growth. Multi-stage filtration including UV-C light inactivates airborne microorganisms.
Choose appropriate coverage for your space. The iAdaptAir 2S purifies 265 sq ft, the 2M handles 530 sq ft, the 2L covers 795 sq ft, and the 2P serves 1,059 sq ft. Complete home purification supports immune system recovery and reduces autoimmune disease triggers.
Mold exposure likely doesn't cause autoimmune diseases in healthy people. However, for those with immune vulnerability, mycotoxins can trigger disease onset or dramatically worsen existing conditions. Protect your immune health with clean indoor air. Shop Air Oasis today and eliminate mold triggers that threaten your wellbeing.