The relationship between diabetes and Chronic Inflammatory Response Syndrome (CIRS) centers on a shared foundation: chronic systemic inflammation that disrupts normal metabolic function. While these conditions may appear distinct, emerging research reveals overlapping inflammatory pathways that suggest important connections worth understanding for those dealing with either condition.
Current scientific evidence indicates that chronic inflammation serves as a common denominator in both diabetes development and CIRS progression. However, it's crucial to distinguish between what research has definitively established versus areas requiring further study.
What Science Shows About Chronic Inflammation in Both Conditions
Diabetes research has firmly established inflammation's central role in disease development and progression. Studies demonstrate that chronic activation of pro-inflammatory pathways contributes to insulin resistance, beta cell dysfunction, and the metabolic abnormalities characteristic of Type 2 diabetes.
The inflammatory markers elevated in diabetes include:
- C-reactive protein (CRP)
- Interleukin-6 (IL-6)
- Tumor necrosis factor-alpha (TNF-α)
- Nuclear factor-kappaB (NF-κB) activation
According to comprehensive diabetes research, these same inflammatory pathways affect multiple organ systems, creating systemic metabolic dysfunction that extends beyond blood sugar control.
CIRS patients often experience similar inflammatory markers, though the triggering mechanisms differ. Mold and biotoxin exposure can activate inflammatory cascades that mirror those seen in diabetes, including cytokine elevation and immune system dysregulation.
Insulin Resistance: A Critical Overlap Point
Insulin resistance represents perhaps the most significant overlap between diabetes and CIRS. While diabetes research has extensively documented insulin resistance mechanisms, emerging clinical observations suggest CIRS patients frequently develop similar metabolic dysfunction.
The inflammatory cytokines elevated in CIRS—particularly IL-1β, TNF-α, and IL-6—are the same molecules that interfere with insulin signaling pathways in diabetes. This shared inflammatory profile may explain why some CIRS patients develop glucose metabolism problems.
Research shows that chronic inflammation can:
- Disrupt insulin receptor function
- Interfere with glucose uptake in muscle and fat tissue
- Promote hepatic glucose production
- Reduce pancreatic beta cell function
For individuals with CIRS experiencing these metabolic changes, understanding diabetes research may provide valuable insights into potential treatment approaches.
The Vitamin D Connection in Both Conditions
Vitamin D deficiency represents another significant overlap between diabetes and CIRS. Diabetes research demonstrates that low vitamin D levels correlate with increased inflammation, insulin resistance, and poor metabolic outcomes.
Clinical observations in CIRS patients frequently reveal vitamin D deficiency, which may contribute to:
- Enhanced inflammatory responses
- Increased mast cell reactivity
- Worsened insulin sensitivity
- Impaired immune regulation
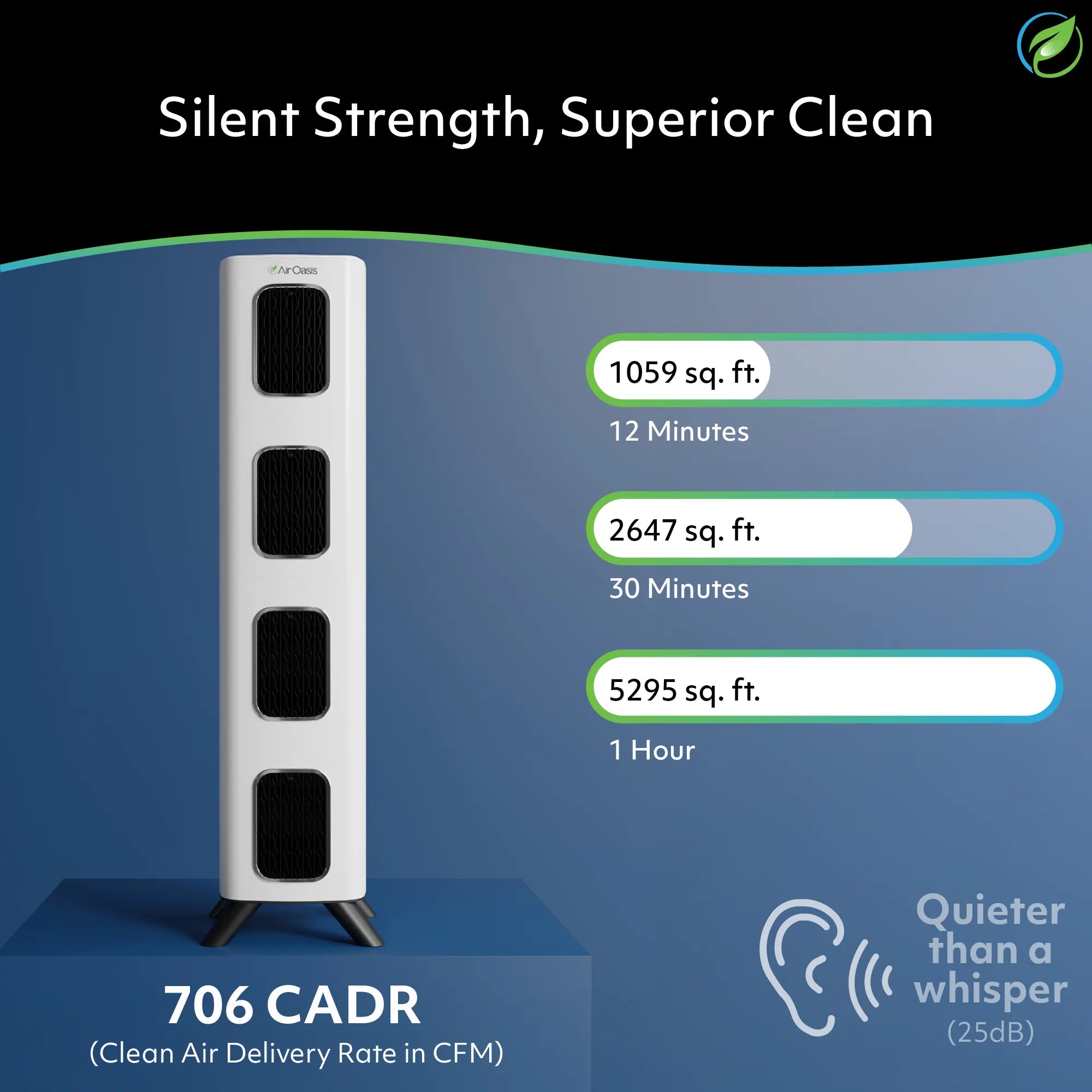
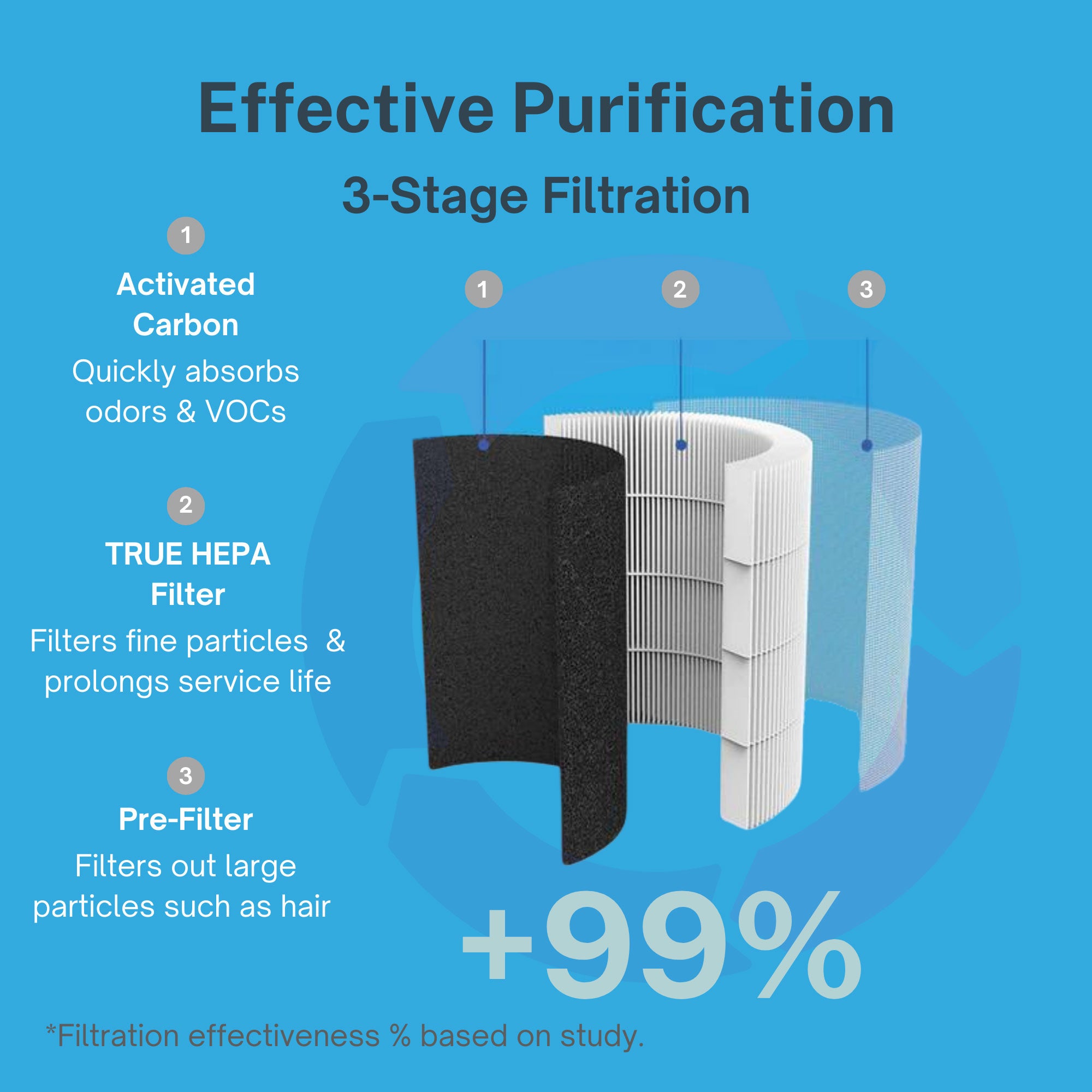
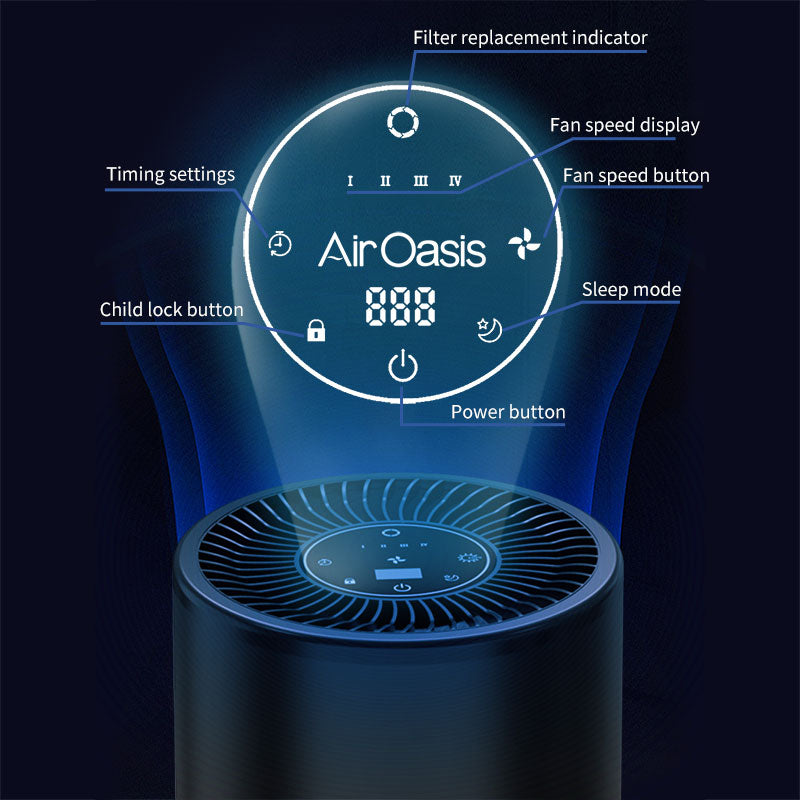
The Air Oasis air purification systems help create cleaner indoor environments that support recovery in both conditions by reducing ongoing inflammatory triggers from airborne contaminants.
Metformin's Anti-Inflammatory Properties: Bridging Treatment Approaches
Metformin, primarily known as a diabetes medication, demonstrates anti-inflammatory effects that may benefit both diabetic and CIRS patients. Research shows metformin can:
- Reduce inflammatory markers including CRP and IL-6
- Activate AMPK pathways that improve cellular energy metabolism
- Decrease pro-inflammatory cytokine production
- Enhance insulin sensitivity through non-glucose mechanisms
Some practitioners report using metformin in CIRS patients experiencing insulin resistance, though this represents off-label use requiring careful medical supervision. The shared inflammatory pathways between conditions suggest potential therapeutic overlap, but more research is needed to establish definitive treatment protocols.
What Current Research Cannot Yet Prove
While inflammatory connections between diabetes and CIRS appear significant, several important limitations exist in current research:
Limited CIRS Research: Most CIRS studies are small-scale or observational, lacking the large randomized controlled trials that establish diabetes treatment standards.
Causation vs. Correlation: While both conditions involve chronic inflammation, direct causal relationships remain unclear. Inflammation may be a shared consequence rather than a connecting mechanism.
Diagnostic Variability: CIRS diagnosis relies on clinical presentation and specialized testing that aren't standardized across medical practice, making research comparison difficult.
Treatment Evidence: While diabetes has extensive treatment research, CIRS interventions lack similar evidence-based validation.
Environmental Controls: A Science-Based Approach for Both Conditions
Both diabetes and CIRS research emphasize environmental factors in disease development and management. Creating cleaner indoor environments supports health in both conditions by:
- Reducing inflammatory triggers
- Minimizing ongoing toxic exposures
- Supporting immune system recovery
- Improving overall health outcomes
The Air Oasis air purification technology provides medical-grade filtration that addresses environmental factors relevant to both diabetic and CIRS patients, including mold spores, volatile organic compounds, and other inflammatory triggers.
Current State of Scientific Understanding
Based on available research, the diabetes-CIRS connection appears to center on shared inflammatory pathways rather than direct disease relationships. Key findings include:
Established Connections:
- Both conditions involve chronic systemic inflammation
- Similar inflammatory markers are elevated in both
- Insulin resistance can develop in both conditions
- Environmental factors influence both disease processes
Areas Requiring Further Research:
- Direct causal relationships between conditions
- Standardized CIRS diagnostic criteria
- Controlled treatment studies comparing approaches
- Long-term outcome data in CIRS patients
Clinical Implications and Future Directions
For healthcare providers and patients, understanding these inflammatory connections offers several practical insights:
- Metabolic Monitoring: CIRS patients may benefit from diabetes-style metabolic monitoring, including glucose and insulin levels.
- Anti-Inflammatory Approaches: Treatments effective for diabetic inflammation may have applications in CIRS management.
- Environmental Controls: Both conditions benefit from reducing inflammatory environmental exposures.
- Comprehensive Care: Addressing vitamin D deficiency, insulin resistance, and inflammation may benefit both conditions.
The Bottom Line on Diabetes-CIRS Connections
Current research reveals significant overlap in the inflammatory pathways underlying diabetes and CIRS, particularly regarding insulin resistance and metabolic dysfunction. While these connections suggest potential therapeutic approaches, more rigorous research is needed to establish definitive treatment protocols.
The shared emphasis on reducing chronic inflammation and environmental triggers provides a science-based foundation for supporting health in both conditions. Professional air purification, proper nutrition, and comprehensive medical care addressing inflammatory processes offer evidence-based approaches that benefit both diabetic and CIRS patients.
Ready to address environmental factors that may contribute to chronic inflammation? Shop Air Oasis today for medical-grade air purification systems that help create cleaner, healthier indoor environments supporting recovery from inflammatory conditions.